Adjacent Organ Invasion
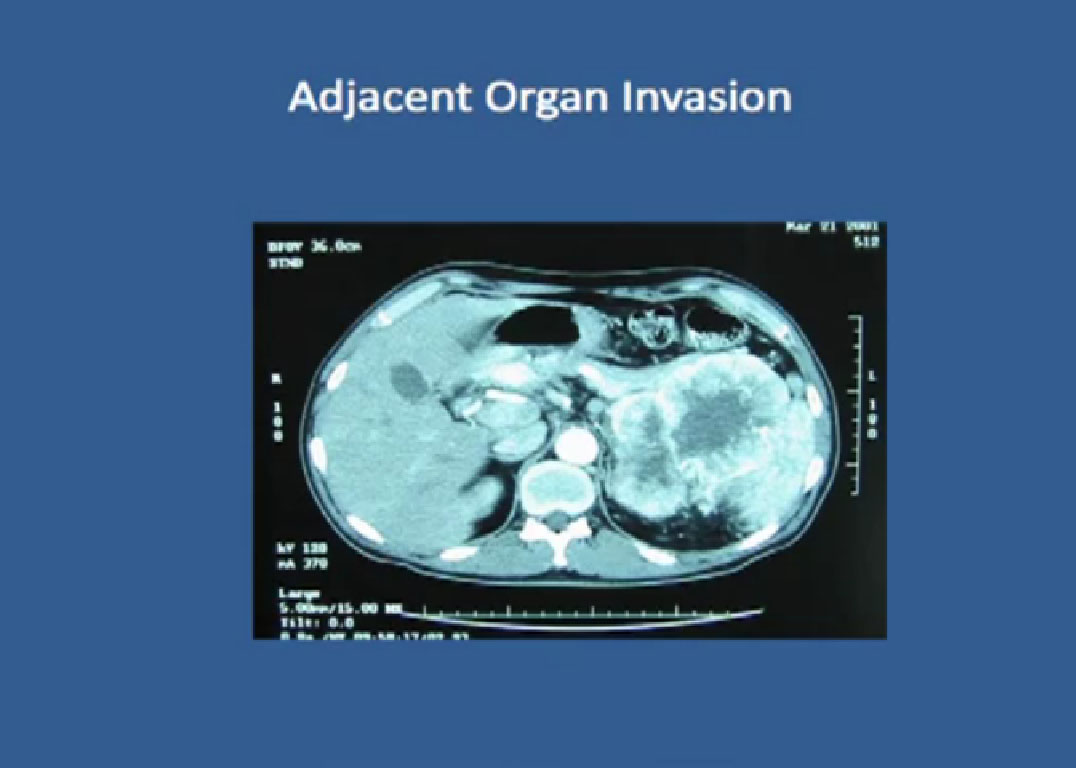 “Little about adjacent organ invasion. Most times when kidney cancer grows, it pushes things away. It rarely invades the liver, the colon, but if so, it is a really bad sign. Where there is locally advanced disease, with local organ invasion, those patients do the worst.
“Little about adjacent organ invasion. Most times when kidney cancer grows, it pushes things away. It rarely invades the liver, the colon, but if so, it is a really bad sign. Where there is locally advanced disease, with local organ invasion, those patients do the worst.
One of the challenges as a surgeon when the patient presents with local organ invasion in a CT scan is to determine if it truly exists. If we truly could identity those patients with local organ invasion, we might refer them for systemic treatment with a targeted agent before doing surgery.
We had 53 patients who had evidence on CT scans of adjacent organ invasion, but 30 did not have metastatic disease and 23 did have metastatic disease. Since 38% of those patients did not have adjacent organ invasion, what does that tell you?
That tells you that CT scans and MRIs are not the be all and end all of surgical planning. Those images are wrong 40% of the time. we were wrong, and if we doomed those patients not to get surgical treatment, and go on to get systemic treatment, it makes me wonder what their outcome would have been.
This graph demonstrates that patients who have organ invasion do bad. In the absence of metastatic disease the median survival was 2 years and with metastatic disease the patients were dead within six months.
Slide 52 These are big operations, median blood loss of 2 ½ liters. Like to point that the big blood loss was not my case! But we do see complications with a mortality rate that is acceptable, so we can get patients through the surgery, but it is a big surgery
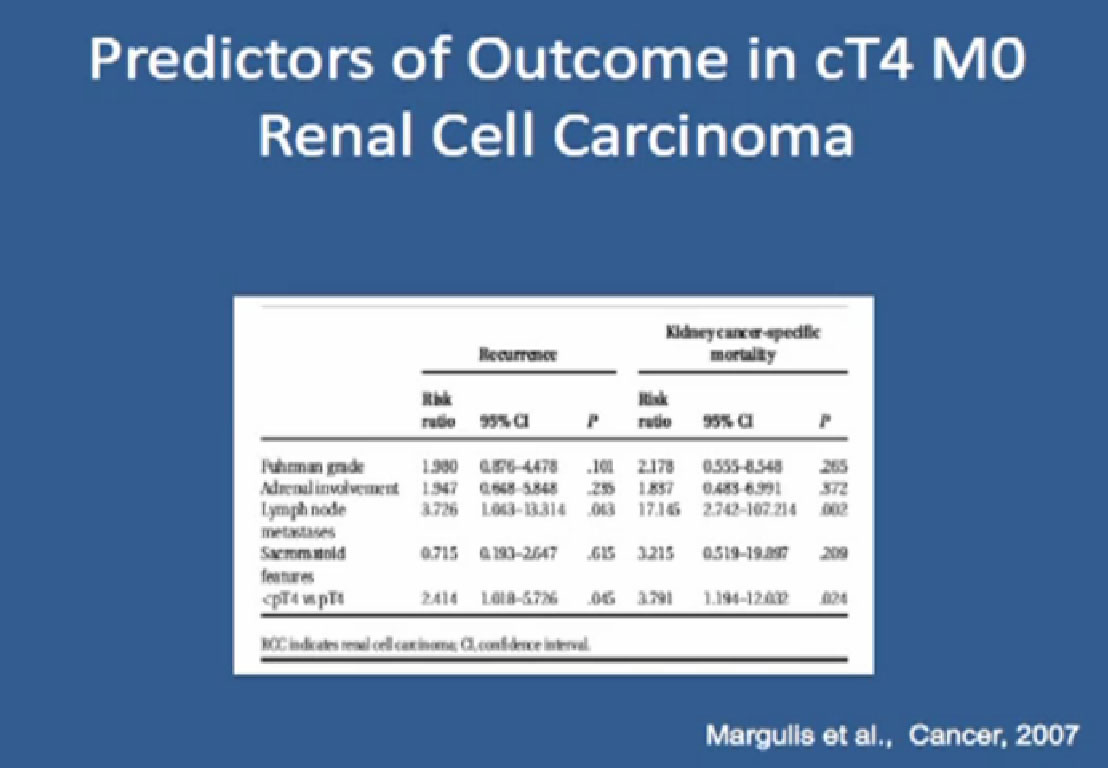
:Again, the factors that predicted outcome for this group — patients who did not have true organ invasion, and again that feature that predicts outcome, presence of node metastases.
Renal Fossa Recurrence
I will finish up with renal fossa recurrence. That means, after the tumor is removed, the patient recovers, the tumor grows back in the same place where the kidney was.
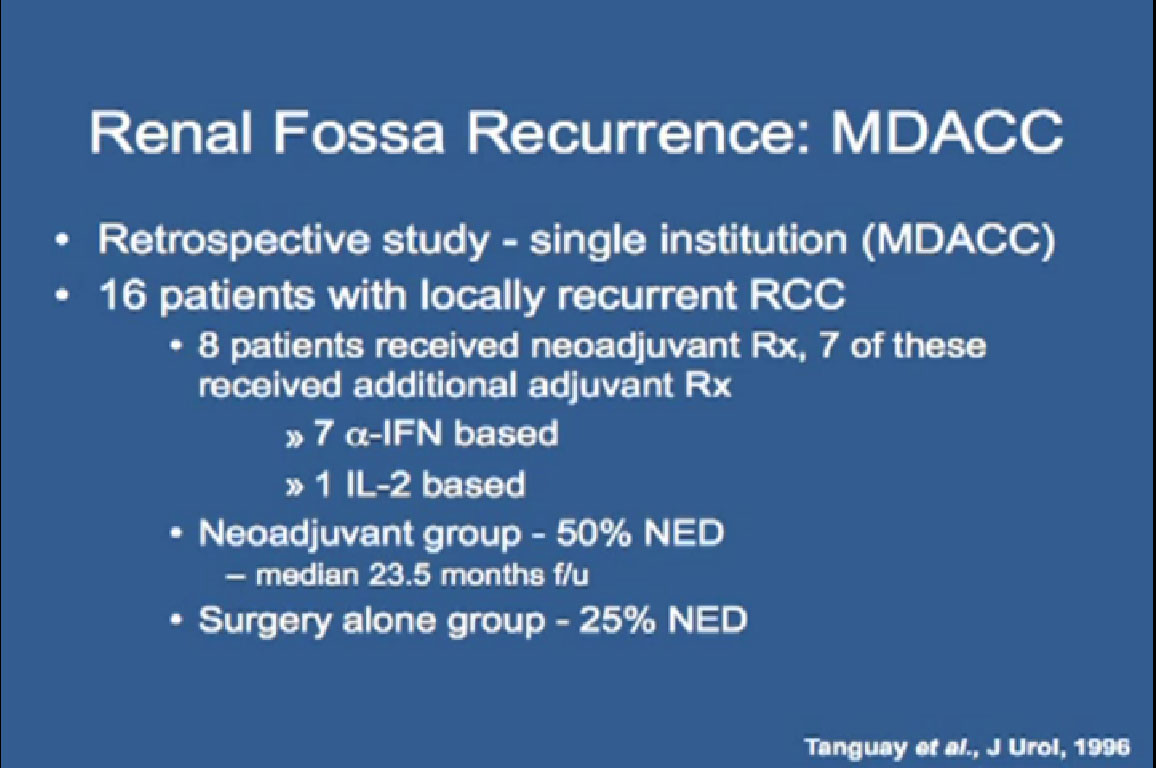
This retrospective study we did at MD Anderson seven years ago looked at 16 patients with locally recurrent RCC. Eight received neoadjuvant therapy and 7 received additional adjuvant treatment after surgery. Of the group of eight with neoadjuvant therapy, 50% were NED. The surgery alone group only 25% were NED, which shows a combination approach, that some form of therapy plus surgery is better than surgery alone.
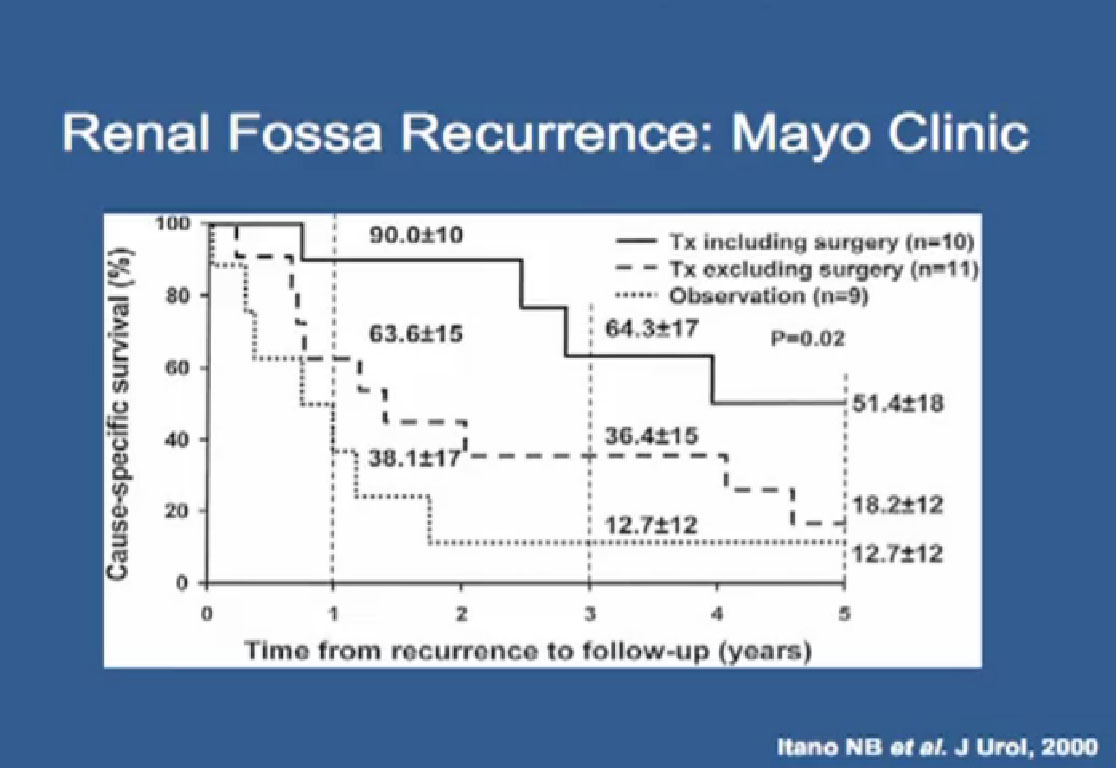 Slide 58:A study out of Mayo Clinic basically shows the same thing. Patients who received surgery and systemic therapy did significantly better than those that received systemic therapy alone.
Slide 58:A study out of Mayo Clinic basically shows the same thing. Patients who received surgery and systemic therapy did significantly better than those that received systemic therapy alone.
 Slide 58: We recently published our study of renal fossa recurrence. We identified 54 patients who present with local recurrence, 69% of these patients received some sort of peri -operative systemic therapy. They all underwent surgical resection.
Slide 58: We recently published our study of renal fossa recurrence. We identified 54 patients who present with local recurrence, 69% of these patients received some sort of peri -operative systemic therapy. They all underwent surgical resection.
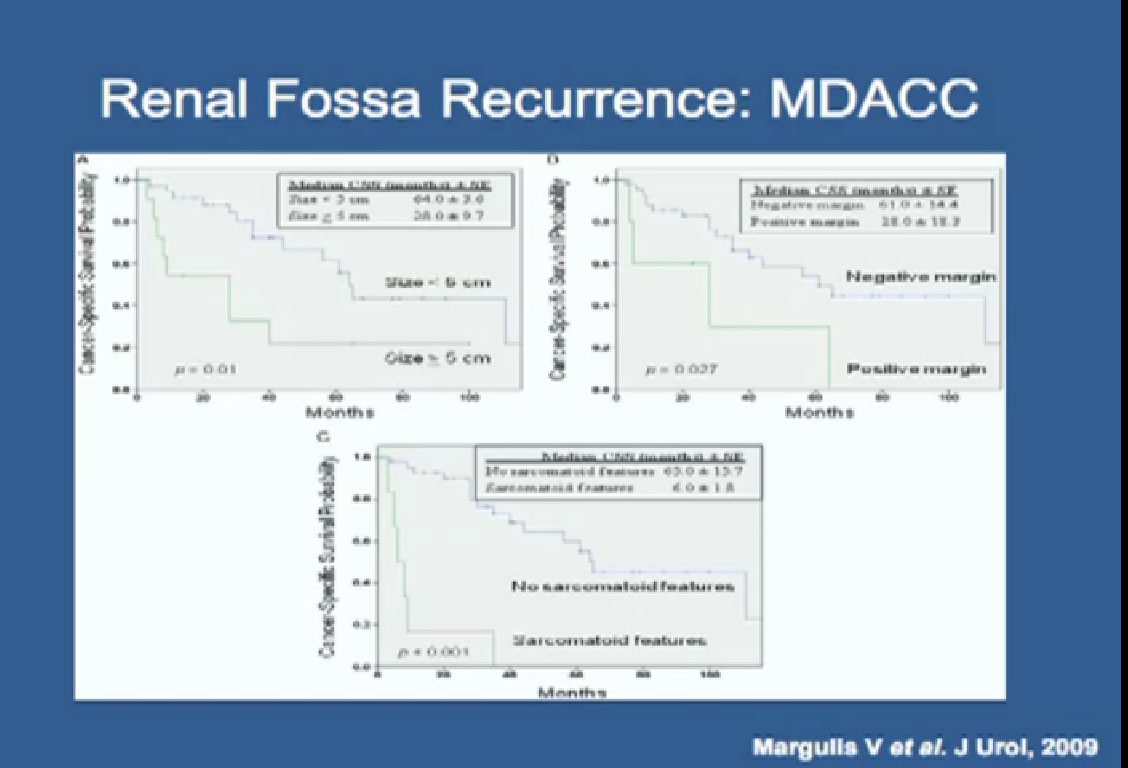
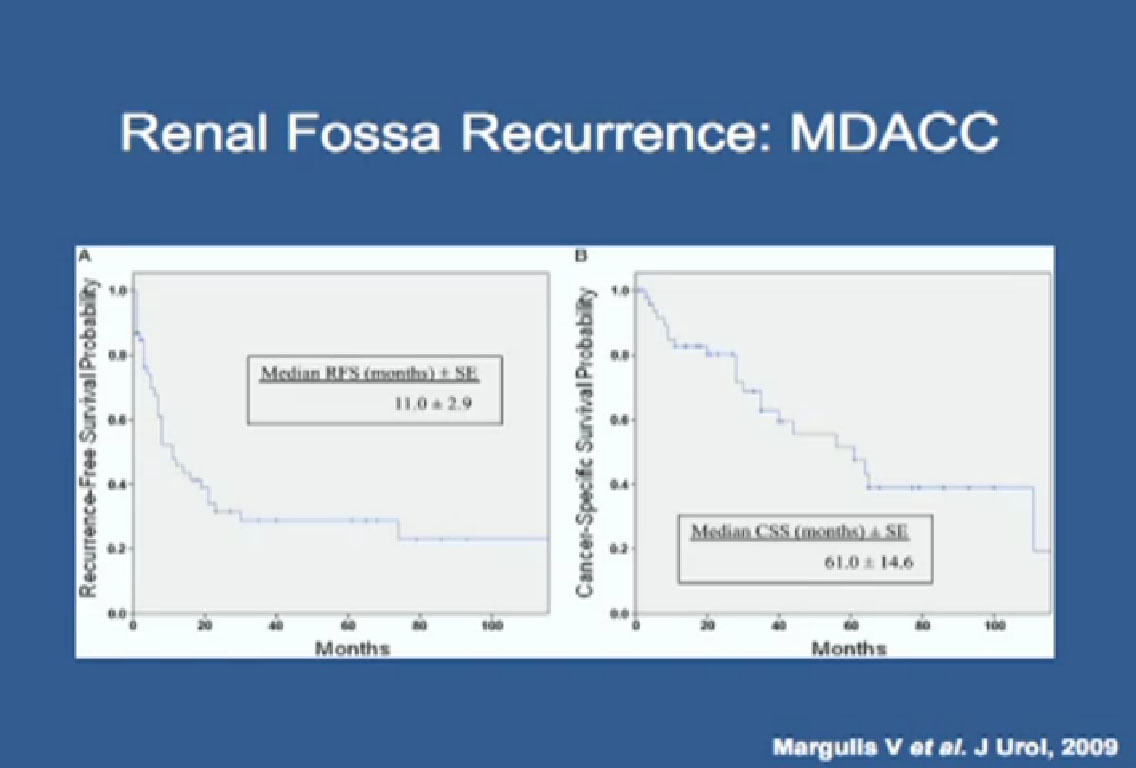 Slide 59: Again, this is a relatively aggressive form of RCC, with the occurrence free survival of about a year, but with aggressive surgical resection, these patients can live a long time. The median cancer-specific survival was more than five years.
Slide 59: Again, this is a relatively aggressive form of RCC, with the occurrence free survival of about a year, but with aggressive surgical resection, these patients can live a long time. The median cancer-specific survival was more than five years.
We tried to identify which features predicted outcome and found that those patients whose tumor size was less than 5 cm, and the ability to get a negative margin,meaning to remove the entire tumor with surgery– the absence of sarcomatoid features, a normal level of LDH in the blood test and a normal alkaline phosphatase, blood tests that we get; all these features predict outcome.
Nowadays when someone presents with a local renal fossa recurrence, we look at these features to see whether or not they are a good candidate for surgery, or if we should refer them to our medical oncologists for additional treatment.
 Slide 62 is incomplete/ Wood’s comments follow: In summary, aggressive surgical resection, when feasible, still remains the best treatment for renal cell cancer. The role of targeted therapy agents in the adjuvant and neoadjuvant setting is unknown and should be protocol driven. Management of locally advanced disease remains a surgical challenge, but when done properly and by experienced surgeons, can give excellent outcomes.”
Slide 62 is incomplete/ Wood’s comments follow: In summary, aggressive surgical resection, when feasible, still remains the best treatment for renal cell cancer. The role of targeted therapy agents in the adjuvant and neoadjuvant setting is unknown and should be protocol driven. Management of locally advanced disease remains a surgical challenge, but when done properly and by experienced surgeons, can give excellent outcomes.”
QED