Dr. Chris Wood; MD Anderson Cancer Center
KCA Patient Conference; April 14, 2010
Surgical Management of Locally Advanced Renal Cell Carcinoma Part 3 of 4
Budd-Chiari Syndrome & Nodal Disease
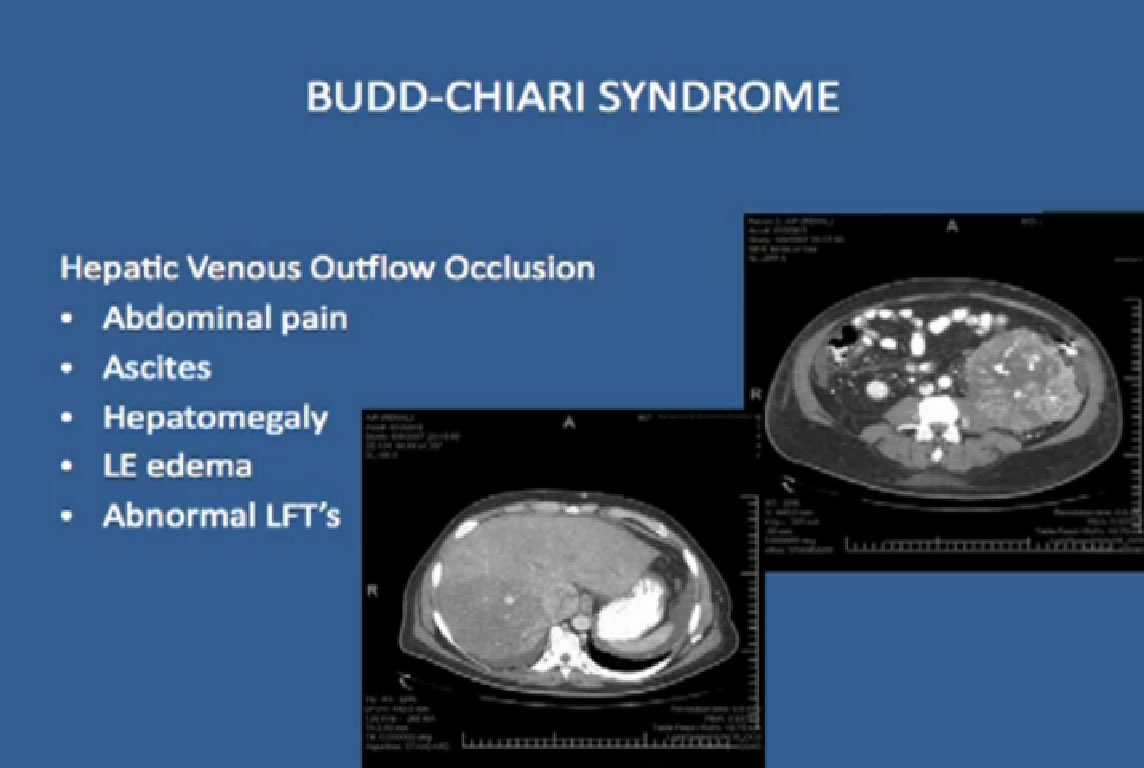
One devastating complications of venous tumor thrombi is the Budd-Chiari Syndome. The thrombus gets so big that it plugs up the vein, plugs up venous outflow from the liver. Patients present with abdominal pain, ascites, i.e., fluid in the abdomen, edema of lower extremities, enlarged liver, and their liver function tests are all abnormal.
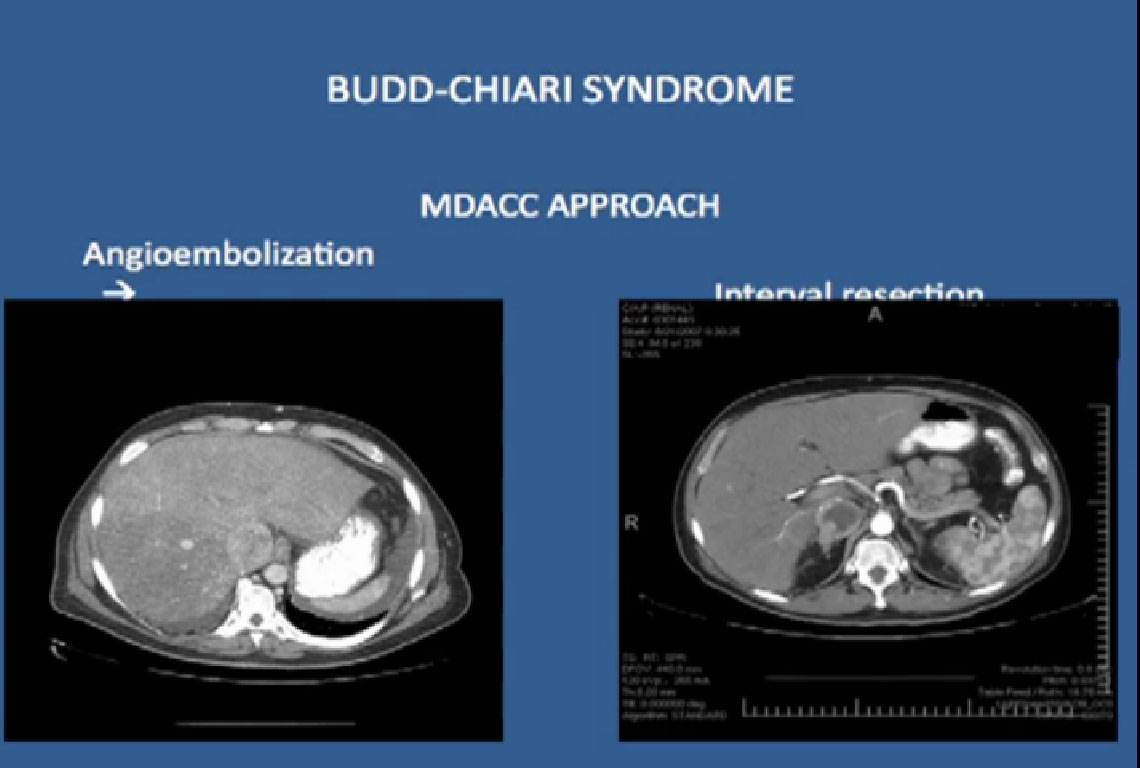
If we take these patients to the operating room, the mortality rate is about 80%. Because of this we no longer take these patients to the OR Instead we will embolize the tumor, cutting off flow of the blood to the tumor. For those patients that regress, we will take them to surgery and they do well.
It is not a very common presentation; we had six patients, two of whom were without evidence of disease after 3 years, using this approach.
NODAL DISEASE
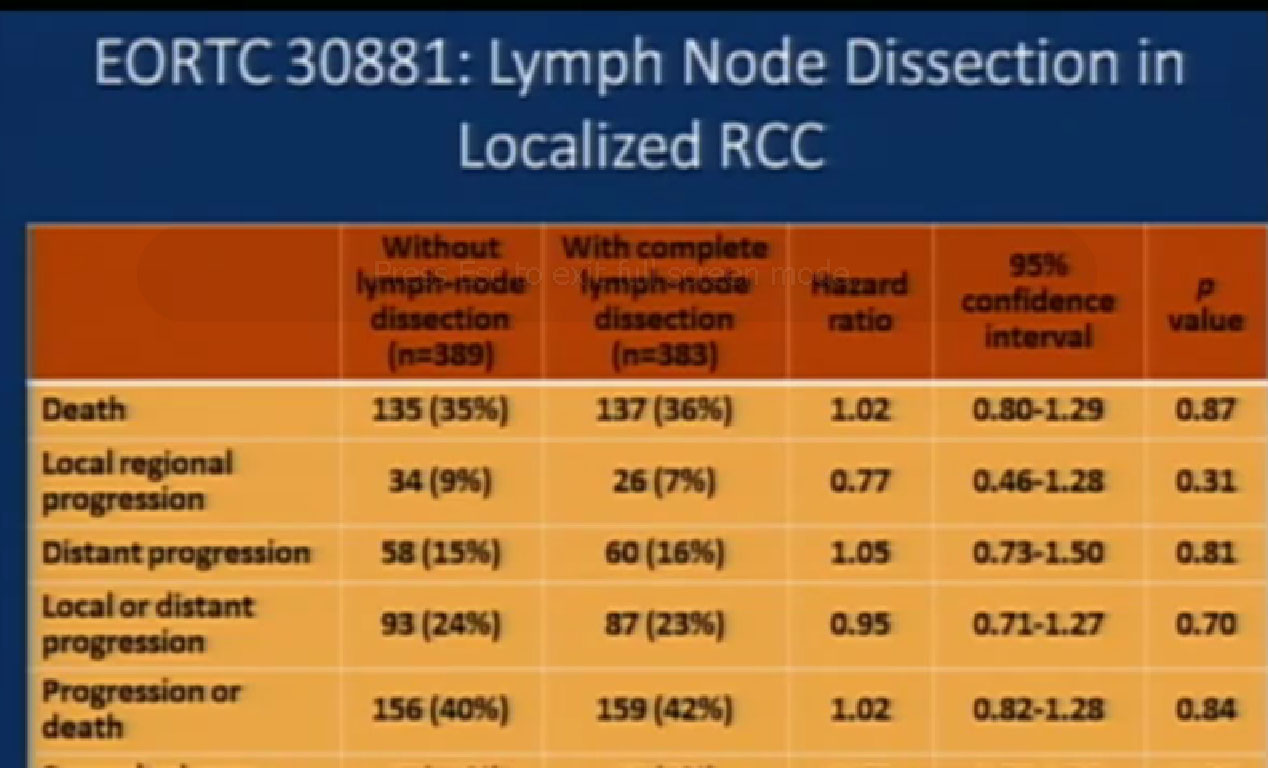
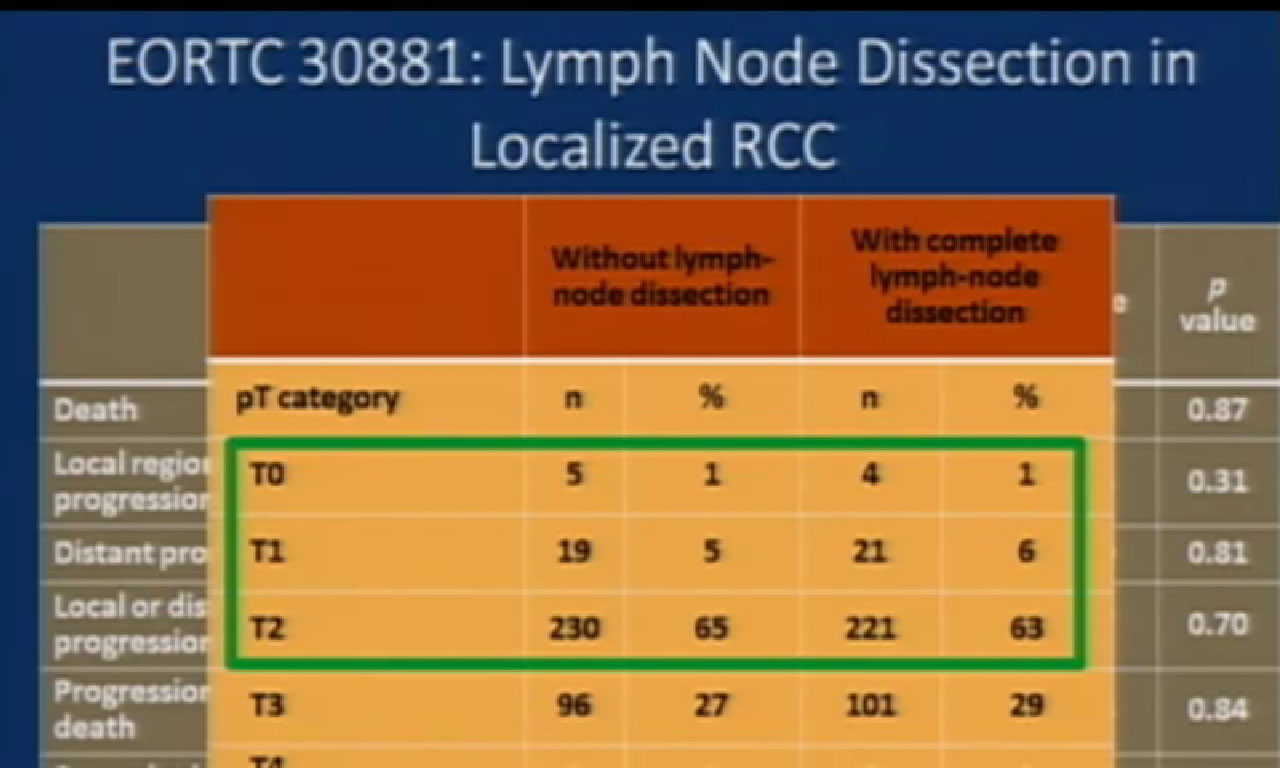
There is a study where patients with localized RCC were randomized to either node dissection or not– to look to see if node dissection improved outcome. This trial showed that patients who had no dissection did no better than those who did not have node dissection. Many will use this in urology community to say that patients who have kidney cancer do not need to undergo node dissection in the absence of metastatic disease.
In a more recent update on this, again, those patients who had a node dissection did no better than those with a node dissection.
But one thing about this trial that troubles me and many in the urologic community is the significant percentage of patients who had very low stage disease. So it gets to the discussion of risk. If you study what you are doing in a low risk population where the frequency of the percent of expected adverse event is so small, you will never see a difference. The problem with this trial is that they need to focus on more advanced stage disease to see if node dissection really makes a difference with kidney cancer.
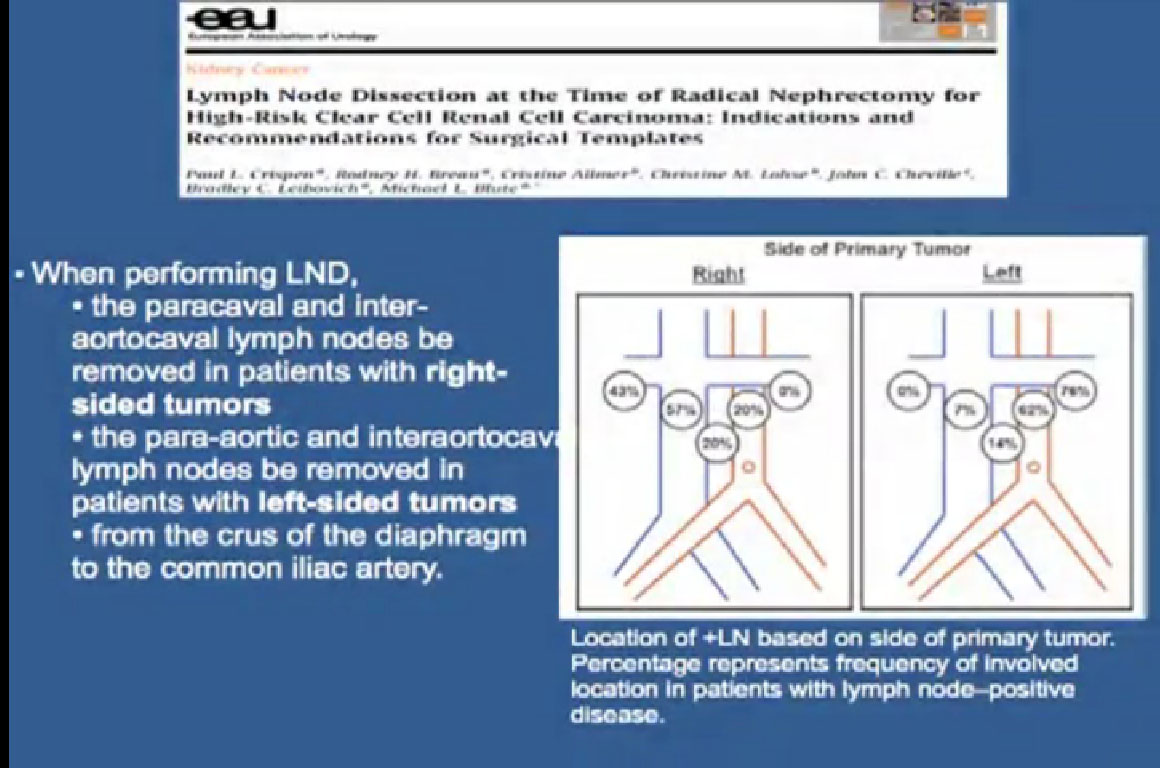 The group at Mayo did some very elegant studies which showed us where the positive nodes are. So now we go in and do a node dissection on a patient with locally advanced tumor, and we have a very defined area where we know the highest likelihood of metastatic disease is to occur. If we took out all the nodes, the complications would be enormous. We now are directed in where we go looking for nodes and remove them in that fashion.
The group at Mayo did some very elegant studies which showed us where the positive nodes are. So now we go in and do a node dissection on a patient with locally advanced tumor, and we have a very defined area where we know the highest likelihood of metastatic disease is to occur. If we took out all the nodes, the complications would be enormous. We now are directed in where we go looking for nodes and remove them in that fashion.
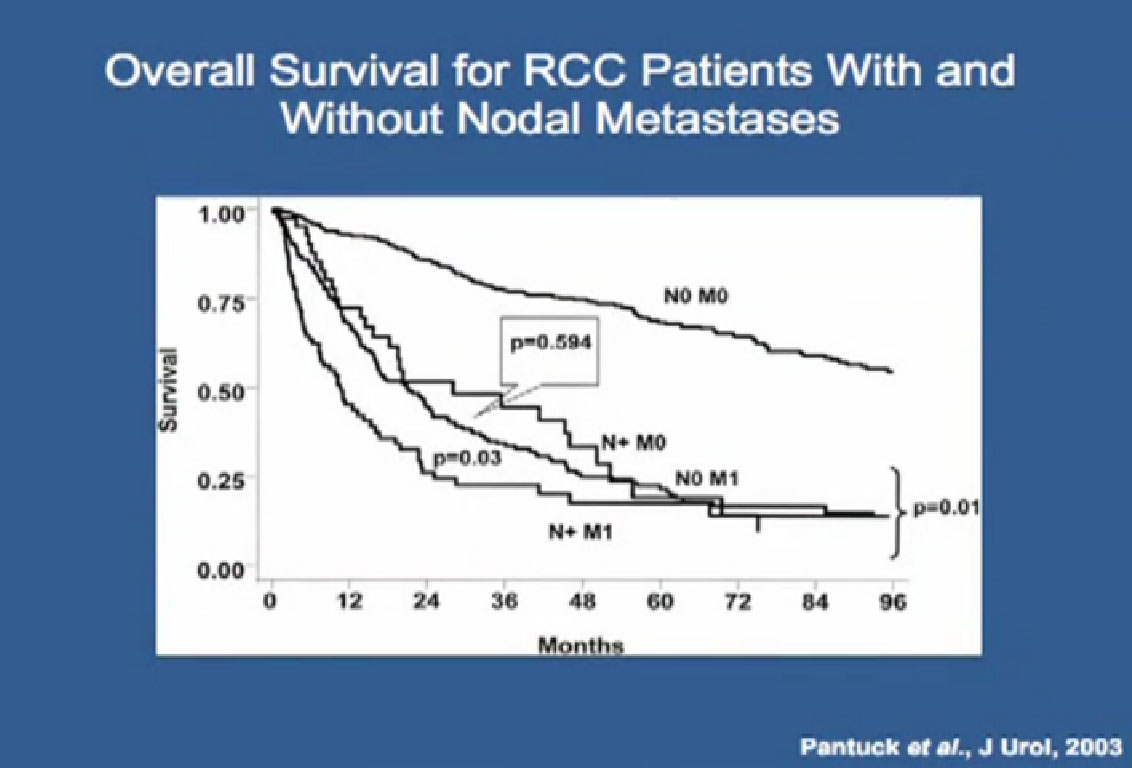
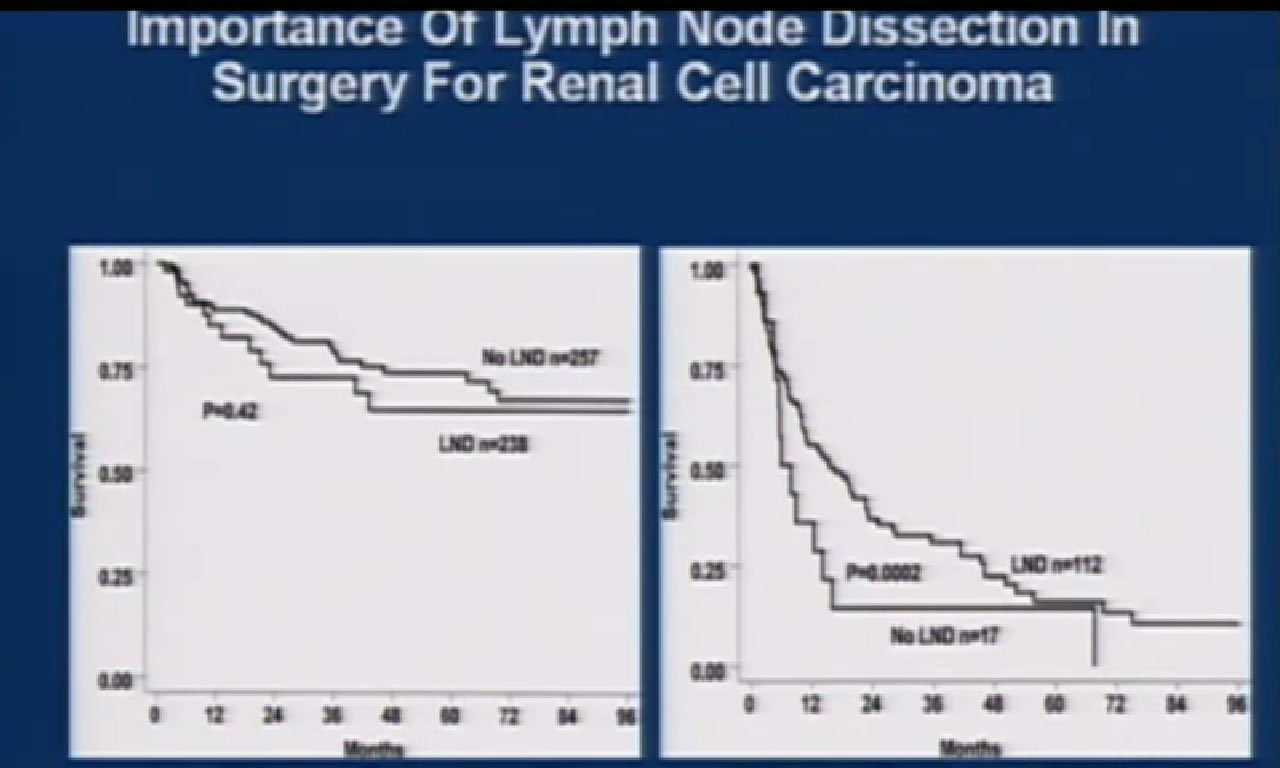 Side 37 : The group at UCLA did a retrospective study and noted that if you did not have enlarged nodes, it did not matter if you took them out or not. Again, like the EORTC trial, but critics of this argue that it presents low stage disease. But one of the interesting things that did notice that in the patients with positive nodes, that if you took those nodes out they did significantly better. Indicating, even in the absence of systemic treatment, surgery could influence the biology of the tumor.
Side 37 : The group at UCLA did a retrospective study and noted that if you did not have enlarged nodes, it did not matter if you took them out or not. Again, like the EORTC trial, but critics of this argue that it presents low stage disease. But one of the interesting things that did notice that in the patients with positive nodes, that if you took those nodes out they did significantly better. Indicating, even in the absence of systemic treatment, surgery could influence the biology of the tumor.
Slide 38
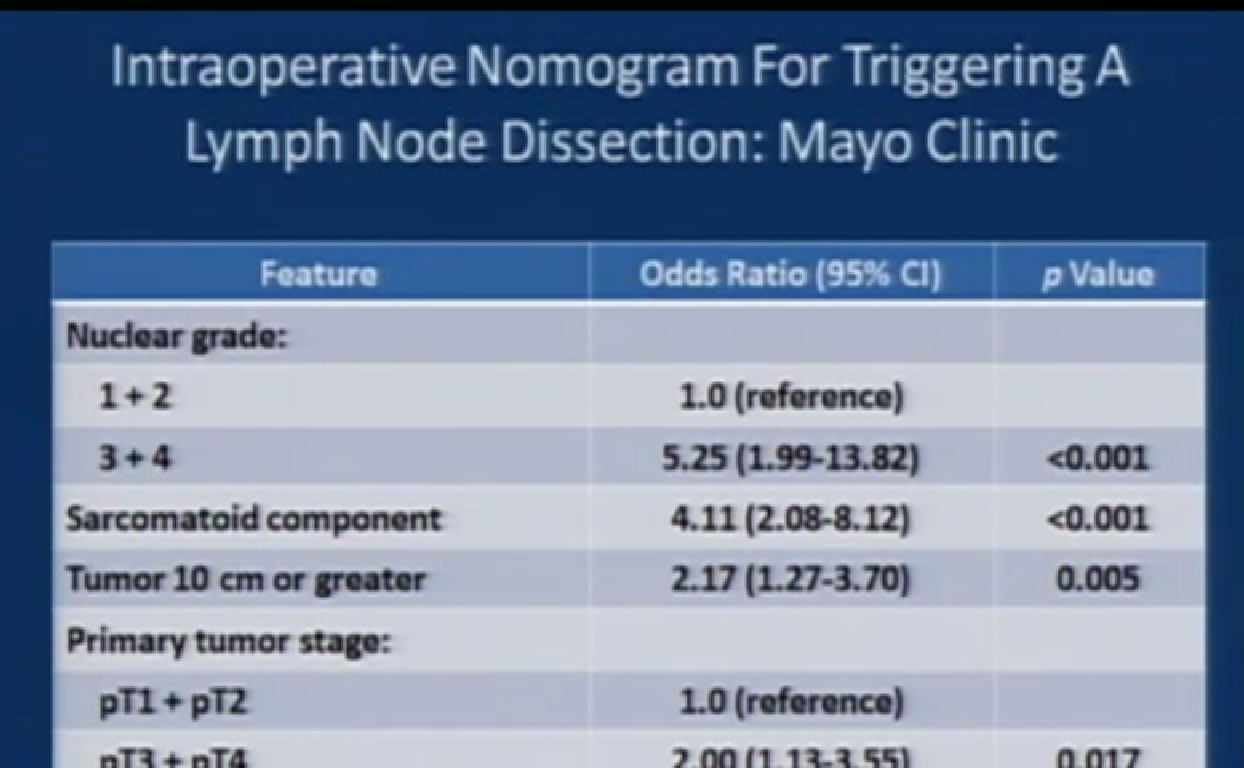
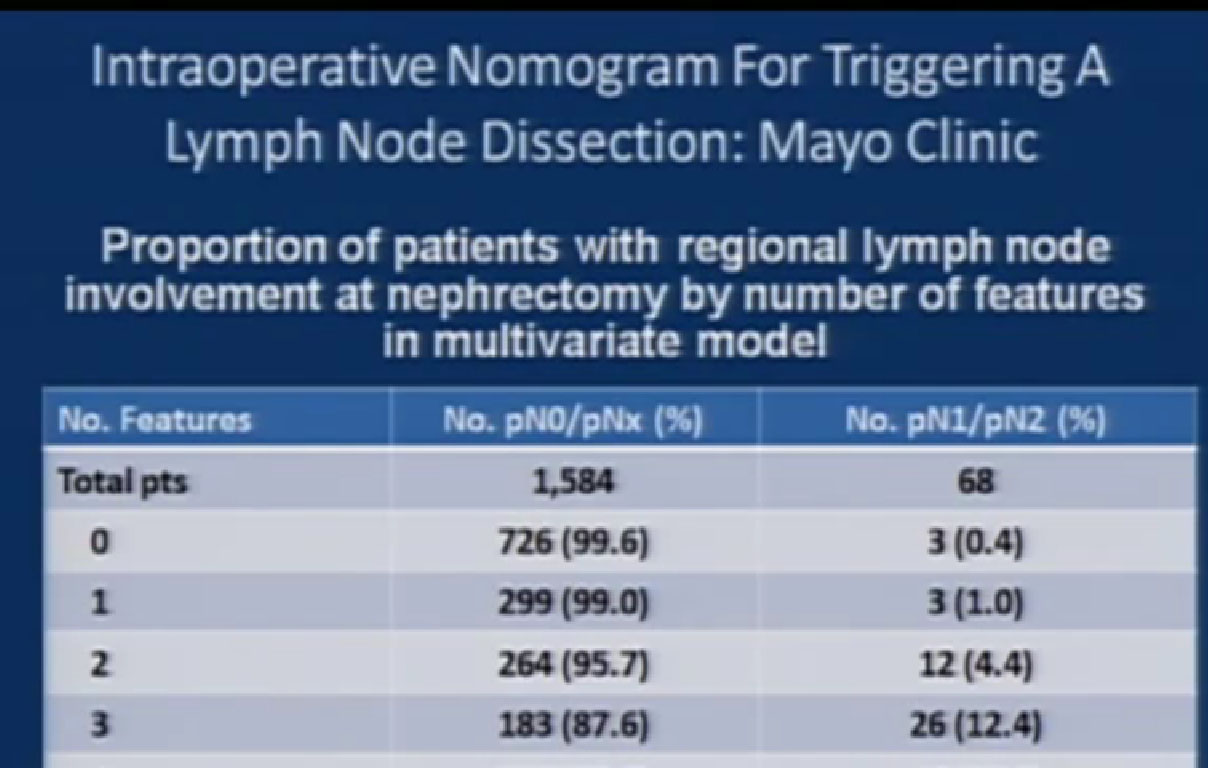
The group from Mayo identified features that predicted for positive nodes. These include high nuclear grade, the presence of sarcomatoid histology, large tumors or more advanced tumors, or the presence of tumor necrosis.
38a They assessed the primary tumor when it came out of the patient, and if there were 2 or 3 of these features, the risk of having nodal disease was significantly high that they triggered a node dissection. Now they use this prospectively to see if this does let us give better outcomes. This may give us the ability to predict who likely has positive nodes and therefore should undergo a node dissection.
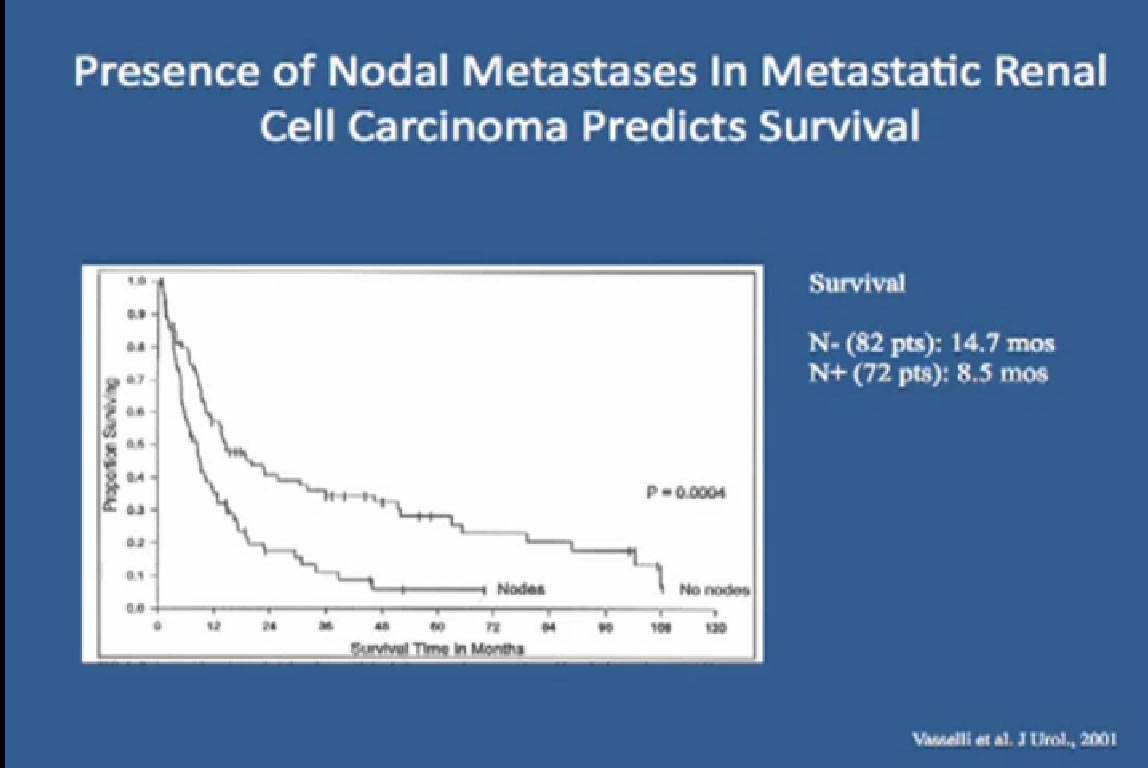
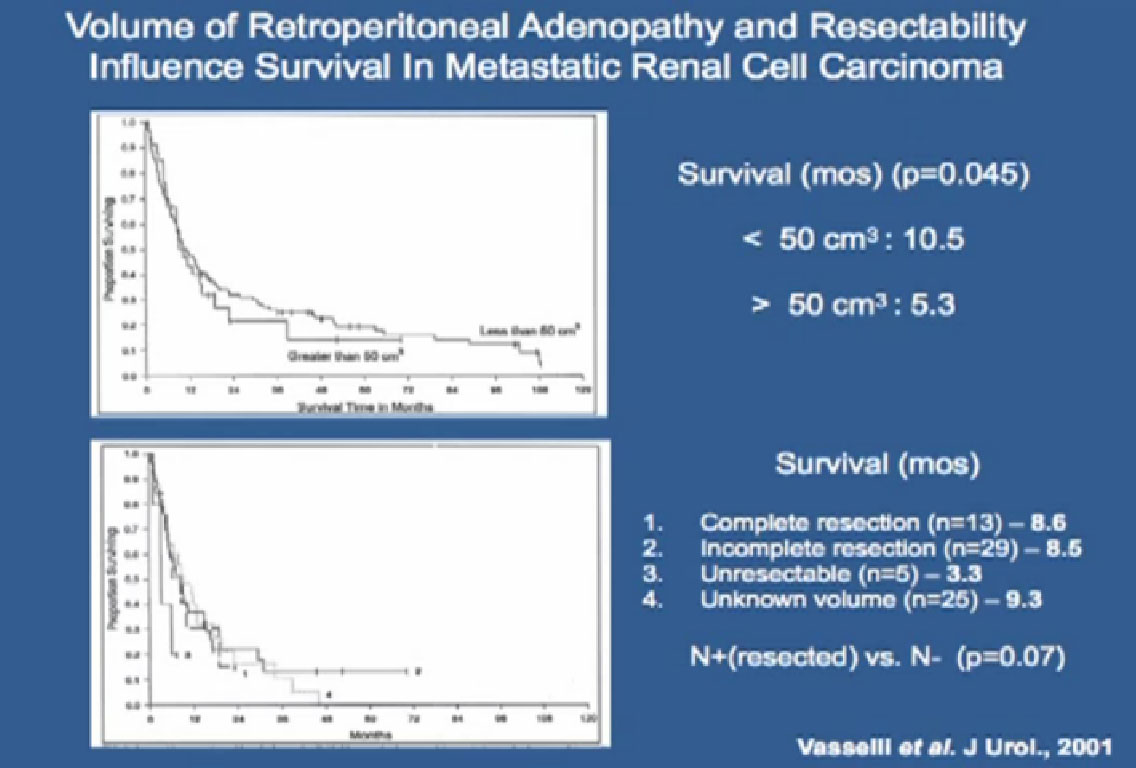
Slide 39 This was a study that was done some years back, but it intrigued me. In patients that had even met and positive nodes, for example, mets to the lungs and positive nodes. Those patients do significantly worse in their prognosis than those without positive nodes. This suggests some adverse biology that is associated with positive node involved.
They also noted that if they could just dissect those nodes, again even in the presence of metastatic disease, they did significantly better than those whose nodes were left in place.
This is a study out of UCLA which shows that patients with metastatic disease do worse in the presence of positive nodes.
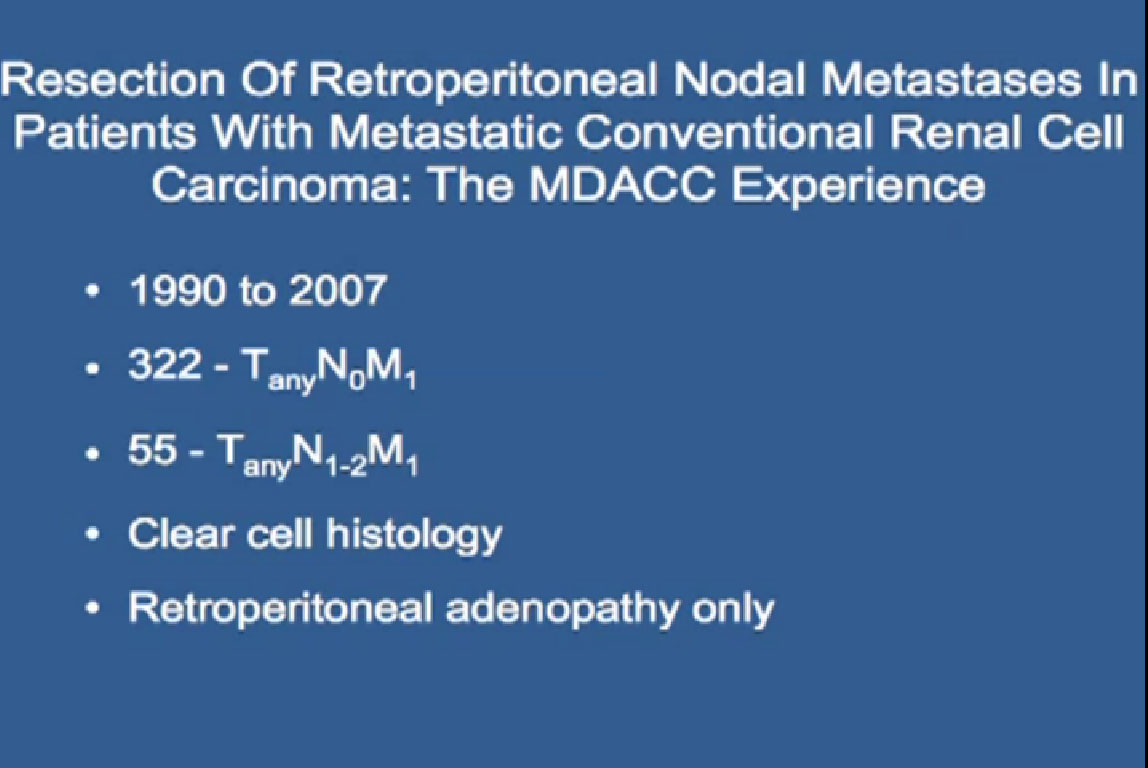
Slide 41a We recently looked at our experience (MDACC) with patients with metastatic RCC and positive nodes, limited to clear cell histology. We had 55 with positive nodes compared to 322 who did not. What we noted that those who present with positive nodes do worse than if they do not have them.
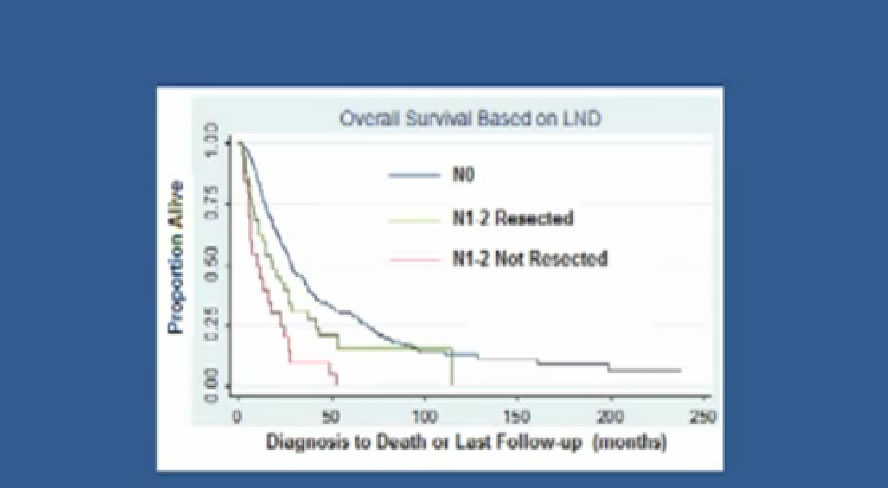 Slide 41b But you can see that if they undergo lymph node dissection, even in setting of metastatic disease, they did significantly better, almost a doubling of their survival as patients who did not.
Slide 41b But you can see that if they undergo lymph node dissection, even in setting of metastatic disease, they did significantly better, almost a doubling of their survival as patients who did not.
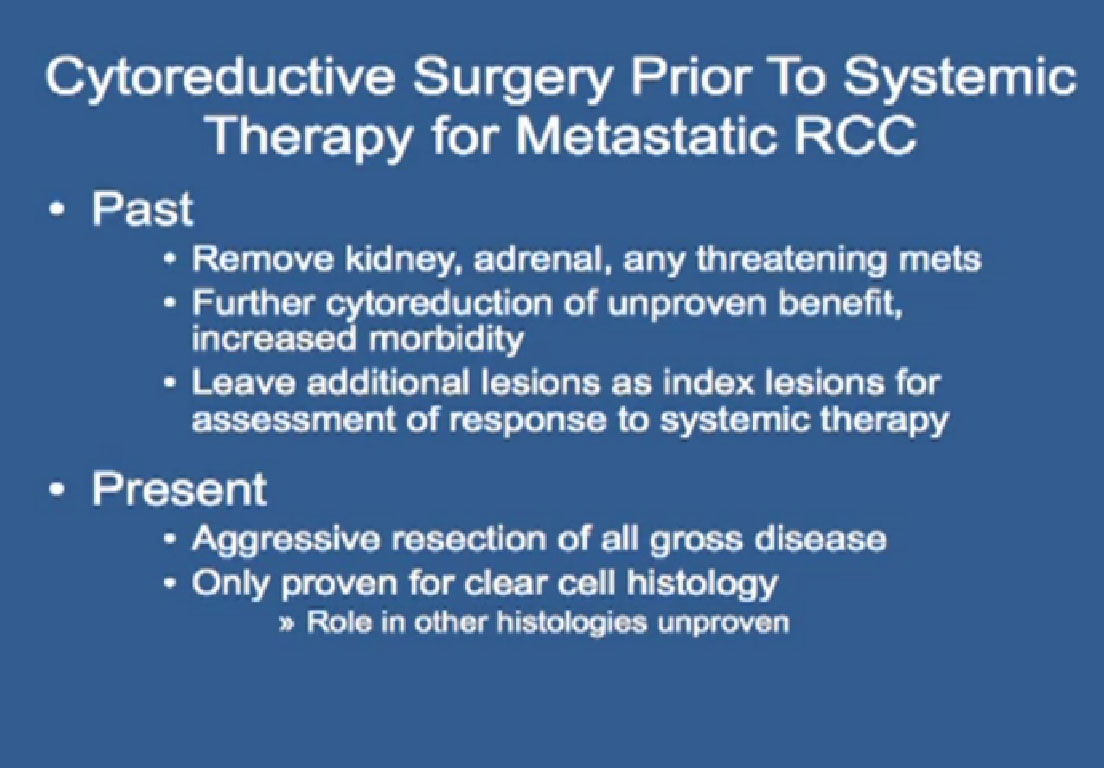 Cytoreductive Surgery Prior to Systemic Therapy for Metastatic RCC
Cytoreductive Surgery Prior to Systemic Therapy for Metastatic RCC
Slide 41c If patients do present with positive nodes, we aggressively resect them, as it significantly impacts on their ability to get treatment. So nowadays, when patients present for cytoreductive nephrectomies, if they have positive nodes, we aggressively resect them, as it significantly impacts their outcome, and their ability to go and get treatment.
Role of Aggressive Surgical Resection in Patients with Positive Nodes in the Absence of Distant Metastases
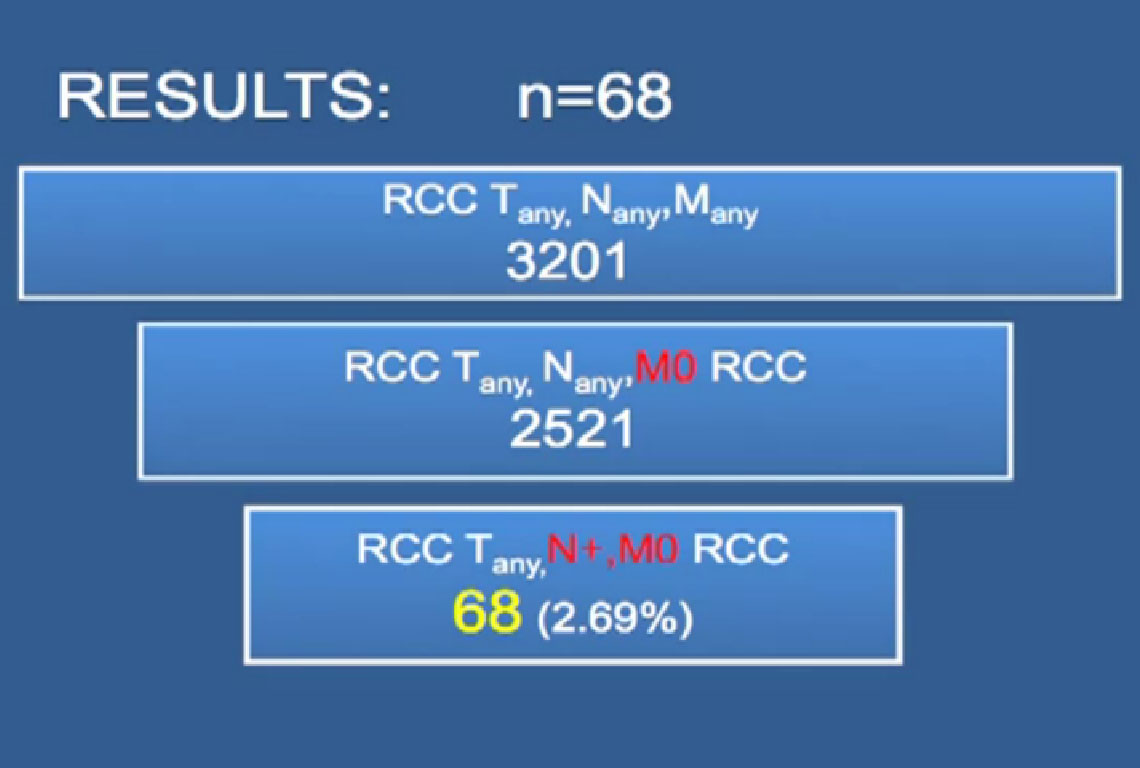
What about those patients that don’t have metastatic disease but just positive nodes. How do those patients do? We recently looked at our series of patients with positive nodes in the absence of distant metastases, and wanted to asses what factors predicted what affected outcome.
Out of 3201 nephrectomies, we identified 2521 who did not have metastatic disease, and of those 68 had positive nodes. Surprisingly, we found, that in positive nodes–that the tumor has left the kidney and metastasized–and surgical patients still do pretty well.
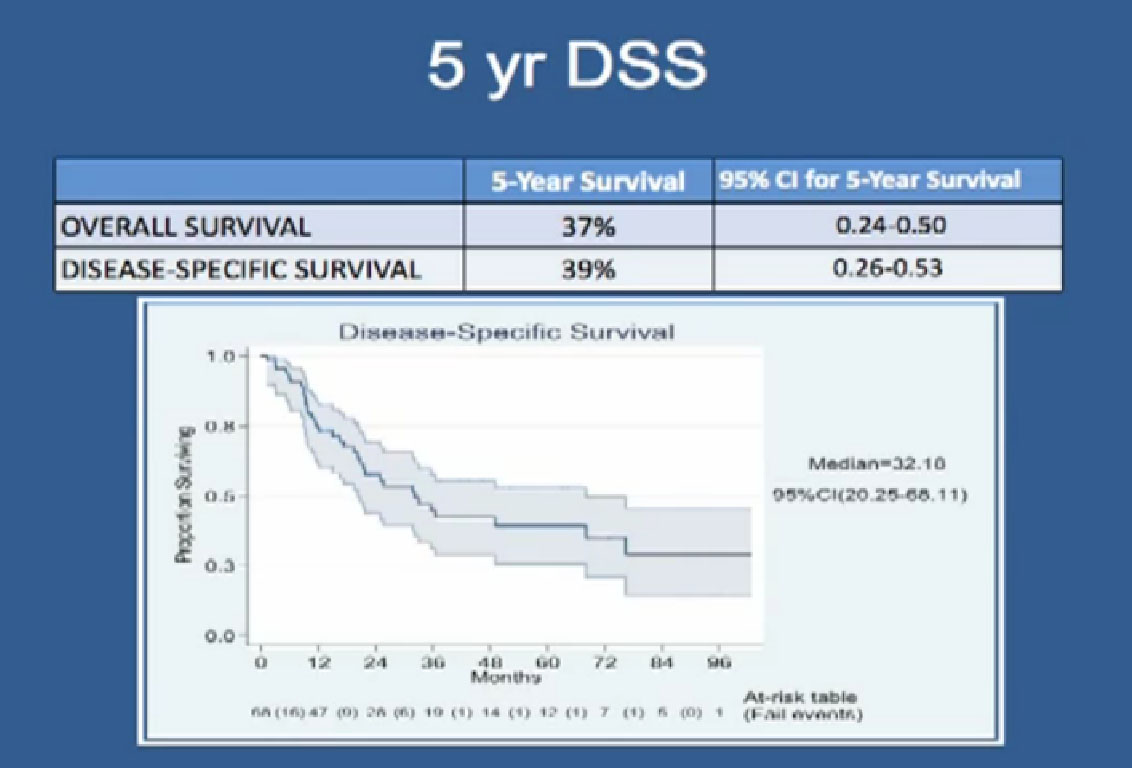 Slide 42: There overall survival rate at five years is 37%. You might say, that is pretty low, but that is with surgery alone. But disease specific survival is 39% at five years.
Slide 42: There overall survival rate at five years is 37%. You might say, that is pretty low, but that is with surgery alone. But disease specific survival is 39% at five years.
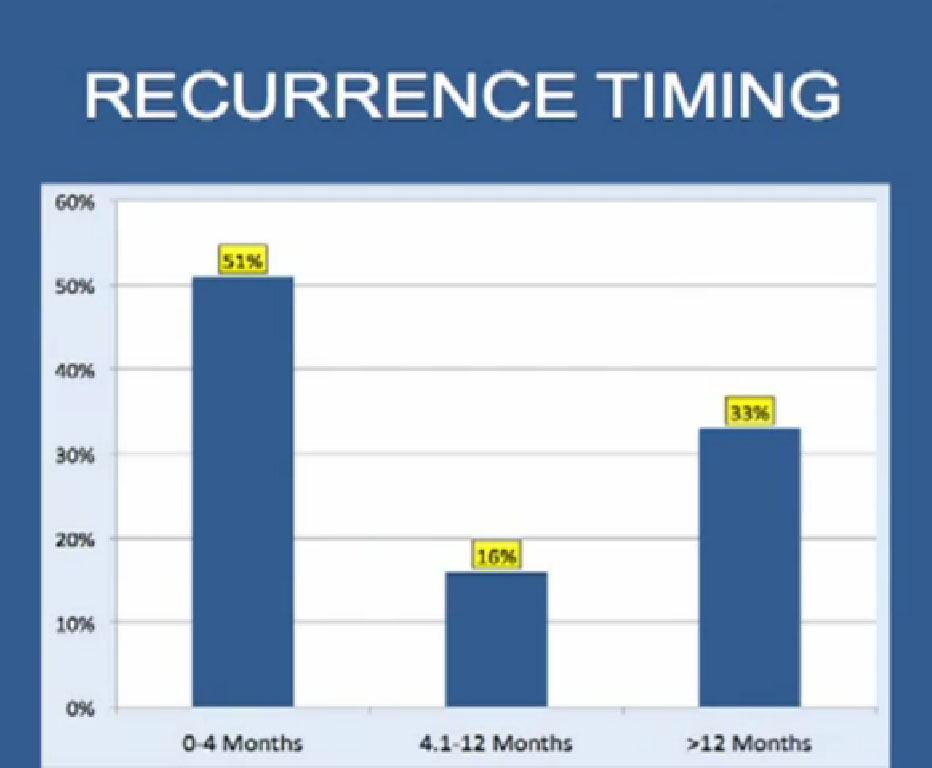
slide44: But when disease recurs, it generally recurs early, at within the first year, but more than a third recur greater than a year out.
Slide 44a: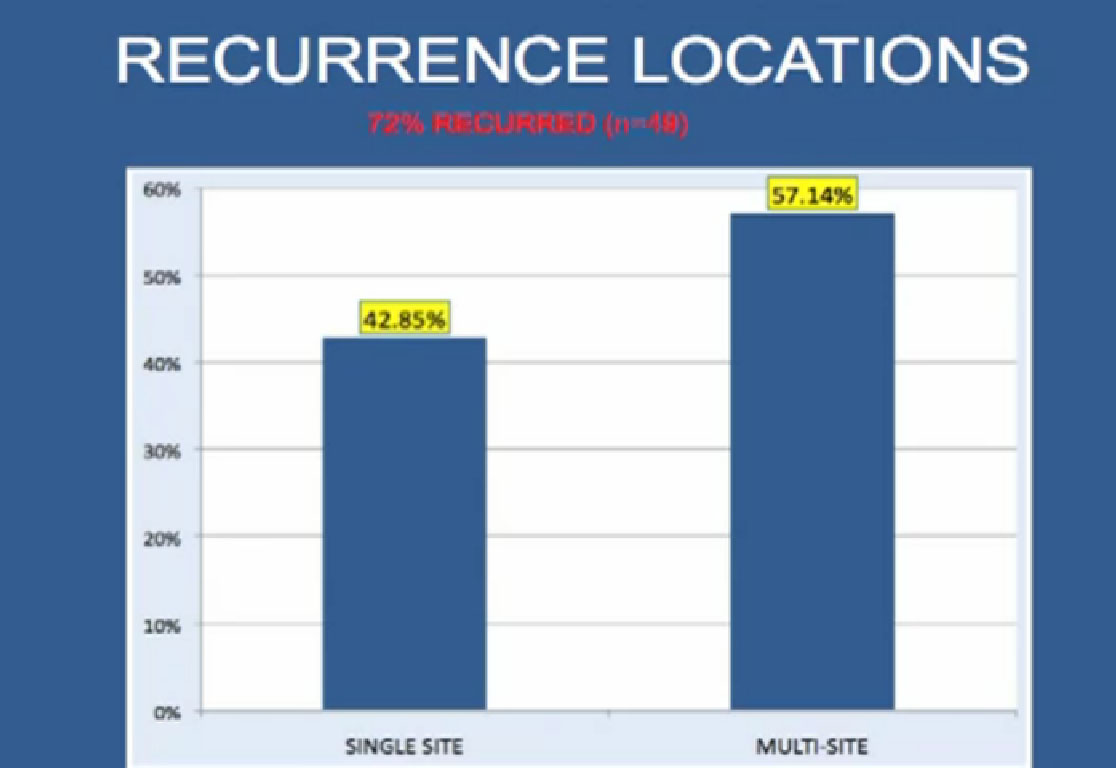 And when patients do recur after this surgery, they usually recur in multiple places with metastatic disease.
And when patients do recur after this surgery, they usually recur in multiple places with metastatic disease.
Slide45
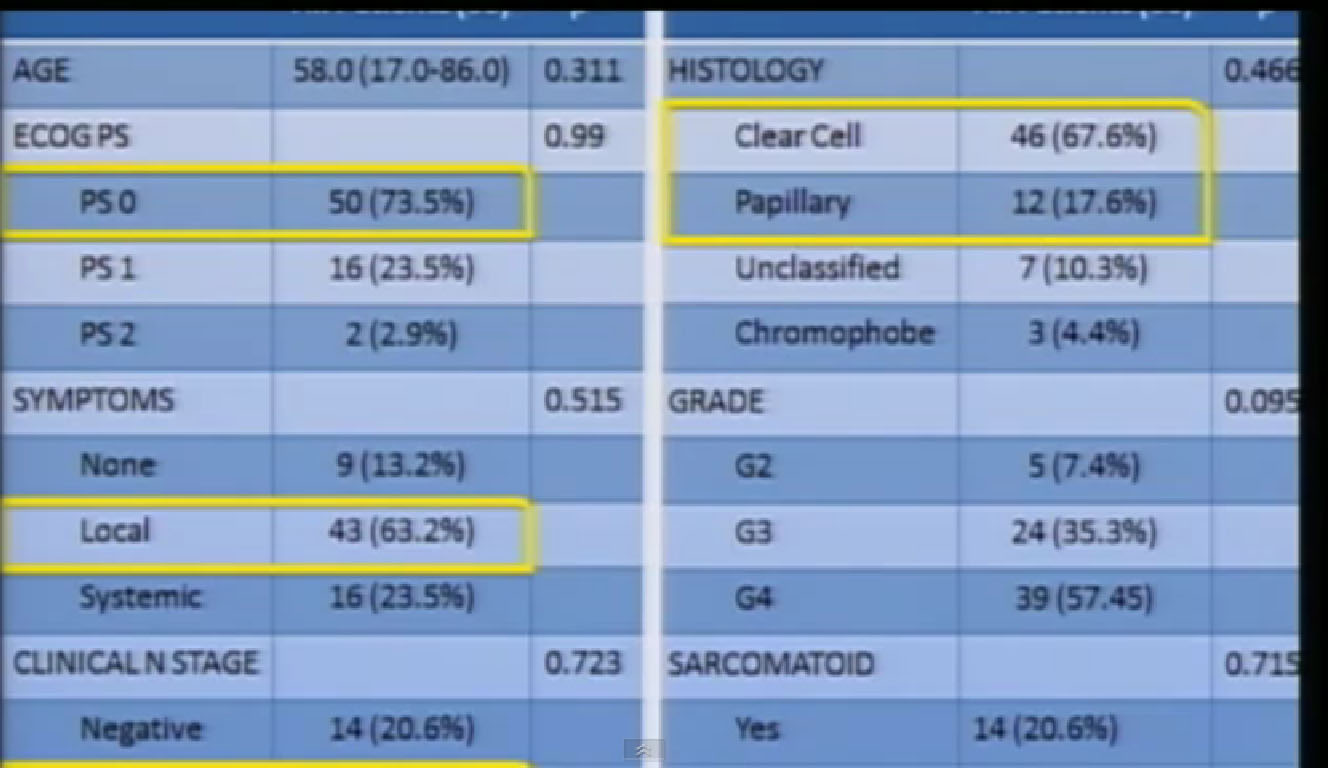
We wanted to look at factors that predicted for outcomes in these patients. So these are these are the demographics, (editor’s note; the video does not include these charts and slide, which are from the original, unedited video) the vast majority had good performance status, they had local disease, confined to the primary tumor and the overwhelming majority had clinically positive disease. This was not microscopic disease, rather big nodes you can see on CT scans.
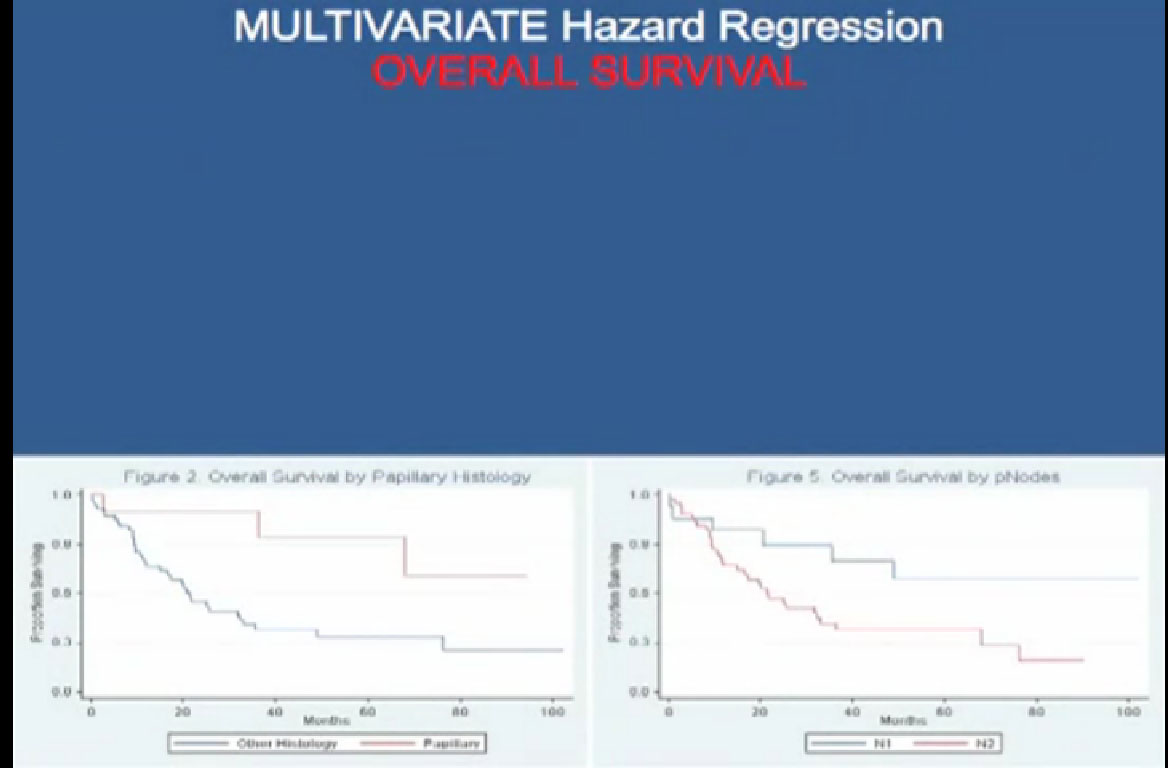
What we noted, interestingly, in terms as predictors of overall survival those patients with papillary histology had a significantly better outcome, than those with clear cell histology. Those with only one node had a significantly better outcome than those with more than one mode.
When we looked at time to recurrence, again, papillary histology seemed to be a predictor of who would do well. So patients with papillary histology and positive node involvement, we will aggressively resect them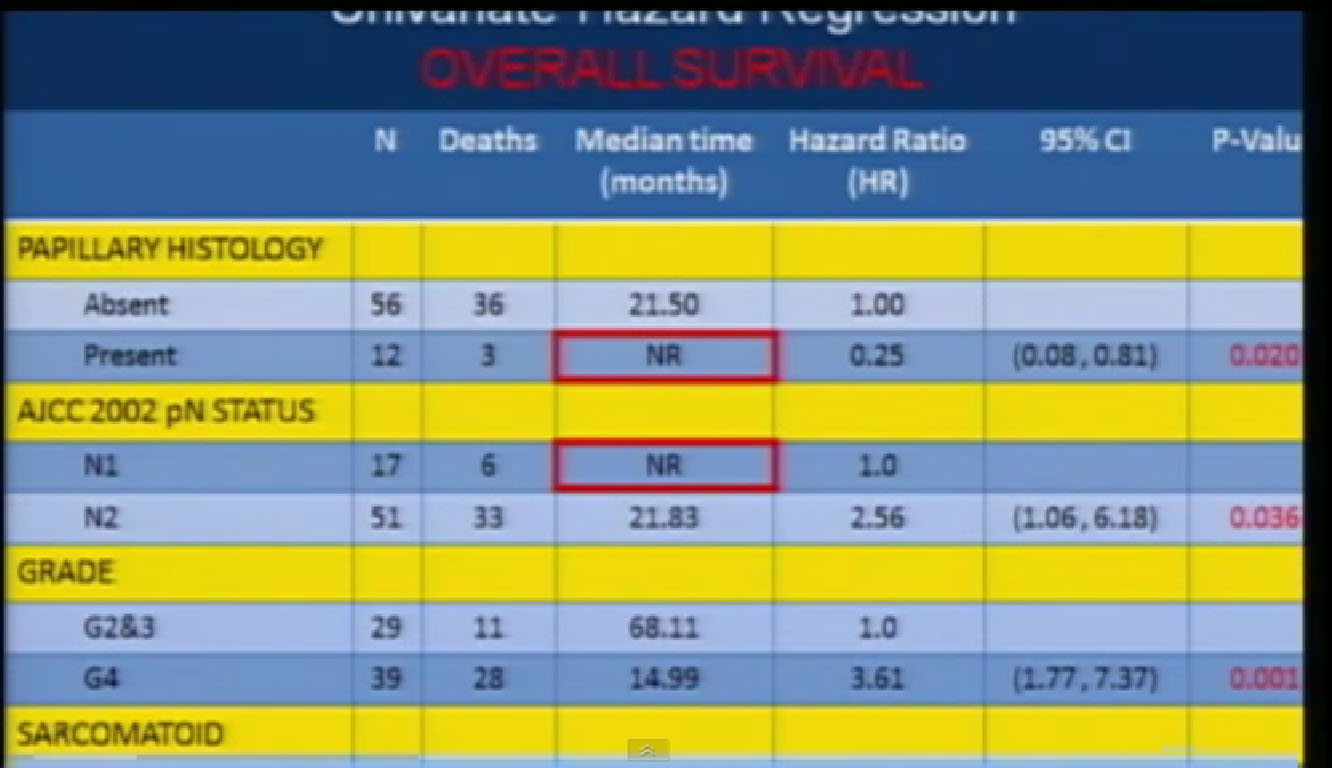 .
.
Slide 45: The multi-variate analysis predicts for overall survival, and papillary histology, the number of nodes positive involved, the presence of sarcomatoid features and status all predicted outcome.
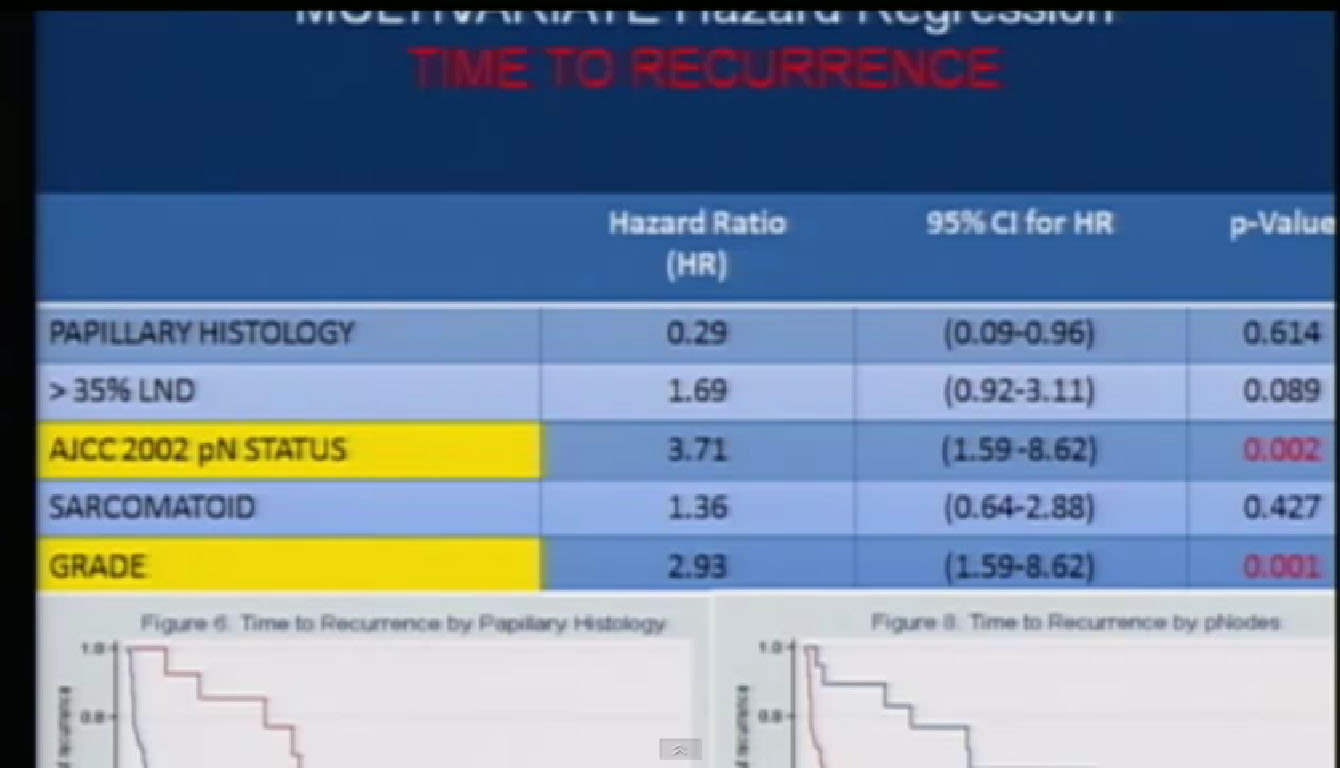 Regards of the time to recurrence, only the number of nodes involved and tumor grade were predictive of outcome in these patients.
Regards of the time to recurrence, only the number of nodes involved and tumor grade were predictive of outcome in these patients.
(Slides are variations of the same information.)
Secondary Treatments
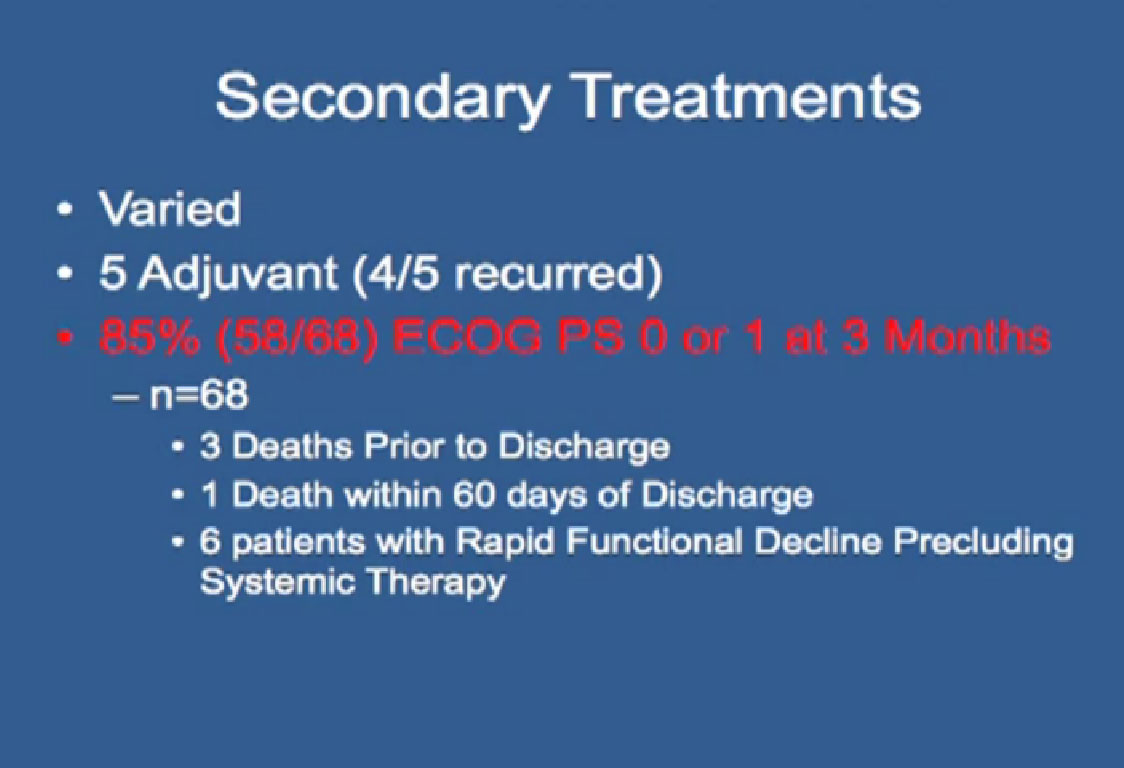 What about adjuvant therapy in these patients? I already told you that adjuvant therapy doesn’t work. In this particular group, 5 got adjuvant ttreatment and in those 4 patients, it recurred. The important thing is that 85% of these patients had good performance status at three months. What does this say? It means we can do an aggressive surgical resection and patients bounce back very quickly. If they need to go on to get additional treatment, even after this very large surgery.
What about adjuvant therapy in these patients? I already told you that adjuvant therapy doesn’t work. In this particular group, 5 got adjuvant ttreatment and in those 4 patients, it recurred. The important thing is that 85% of these patients had good performance status at three months. What does this say? It means we can do an aggressive surgical resection and patients bounce back very quickly. If they need to go on to get additional treatment, even after this very large surgery.
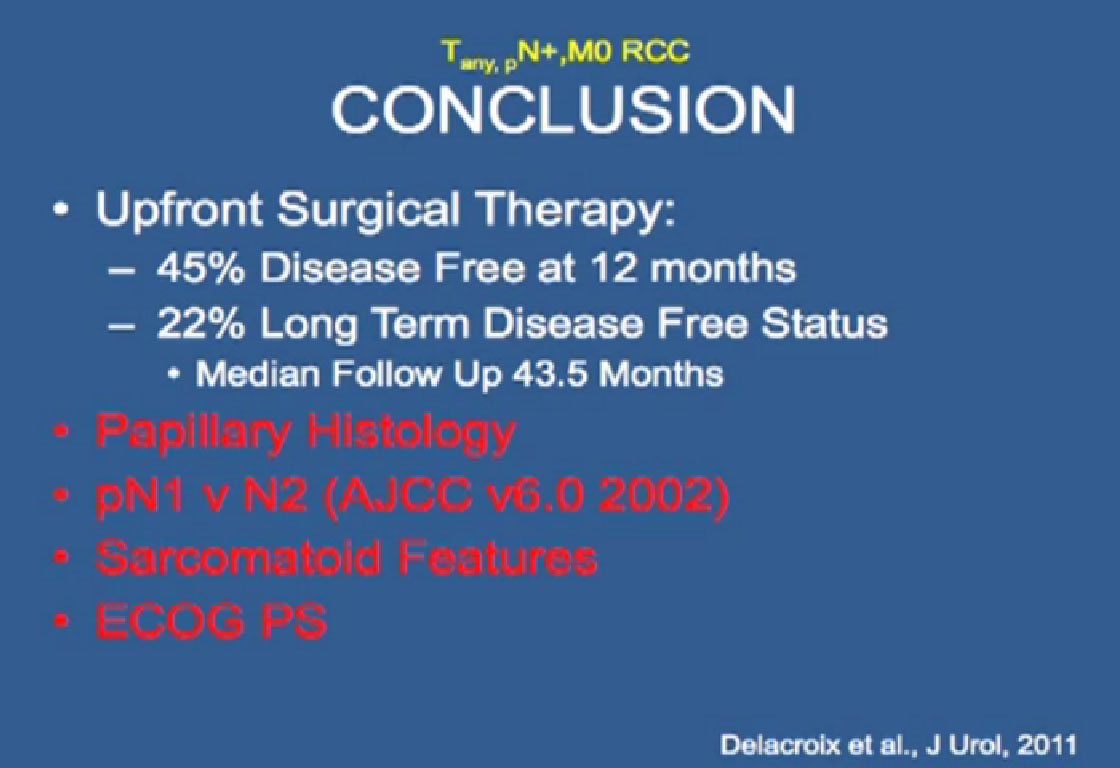 So these are the feature that predict outcome; papillary histology, number of nodes, sarcomatoid features and ECOG performance status.
So these are the feature that predict outcome; papillary histology, number of nodes, sarcomatoid features and ECOG performance status.
I will continue with “Adjacent Organ Invasion” in the next part of the lecture.