Kidney Cancer Association National Patient Conference
Dr. Thomas Hutson, D.O.; Texas Oncology
April 14, 2012
Management of Toxicities Related to Systemic Therapy for Metastatic RCC
Summarized from transcript and video; edited for brevity; Many slides were text-only, so recreated to keep files sizes small. Slides recreated in bold lettering and this font to keep the files small.
To view the lecture, please follow this link; you may copy and paste it into your browser.
http://www.youtube.com/watch?v=KuJoHPA8sww&list=UUv0VRYOltlNQJLCyNMN61Nw&index=45&feature=plpp_video
Be aware that this is a personal summary of the lectures, and that I am not a medical professional; I am a patient, highly motivated to share the information from this KCA conference.
Dr. Hutson thanks the KCA for the conference and begins:
“The “Management of Toxicities Related to Systemic Therapy for Metastatic RCC” is the bane of our existence in RCC; Dr. Jonasch explained the drugs and their benefits earlier, but with benefits often come side effects.
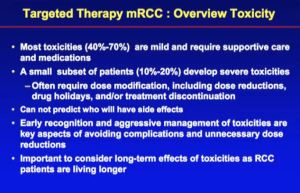
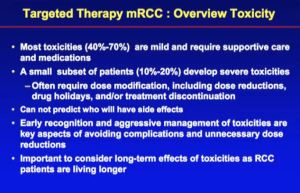
About two-thirds of these side effects–the toxicities–are mild, and are managed by “supportive care”. This means using medications to ease the toxicities. About 1/3 of the toxicities are severe, and may require a dose modification, a dose holiday, stopping the medication for a few days. For most patients, when the medications are stopped, the side effects go away. Most are not permanent. But when toxicity becomes so severe that it affects quality of life, such that we have to withhold that medication, we may move onto another kind of therapy.
Early recognition is very important. I cannot predict if a patient will develop a toxicity and who will not. We think about that from the research perspective, look at it from a genetic perspective. Studies in the medical literature show that patients’ genetics can affect the patients’ toxicity to the drug. Those studies are called pharmacogenomics or pharmacogenetics–things that make an individual patient or a group of patients more susceptible to a toxicity.
These drugs are approved and used around the world and other populations have different toxicities than patients in the US. Asian populations have more severe hematological toxicities, lowering blood counts than we see in US or western European patients. Clearly there is something that is genetic, a so-called pharmogenomic abnormality. Continued research in that area will help us understand that and predict who is going to have those side effects, and let us choose drugs accordingly.
Early recognition of toxicities is the key to avoiding severe toxicities and avoiding dose reductions. When I start patients on these new therapies, I generally see them every 2-3 weeks for a few months. Thus, we can get a handle on side effects, and have a plan, and intervene as needed. Most side effects manifest in first couple of months of therapy, and are often chronic, ongoing. Once we identify them as potential problem for that patient, then we have a strategy. Then I see that patient less frequently, every 4-6 weeks.
I do encourage the doctors–the community oncologists—to do the same, give early aggressive management of the side effect. But the patient or caregiver needs to pick up the phone and call the doctor or doctor’s nurse early when you have a side effect.
We must also consider long-term effects from these side effects, because patients are living longer. With these agents, used in sequence, patients are living 3-5 times longer than they were just a few years ago. Some patients stay on them for years. One man in my practice has been on Sutent for eight years; there are side effects that he will live with for a long time. These therapies have only been available for 5-6 years, and we are just now learning how to utilize them and their toxicities.

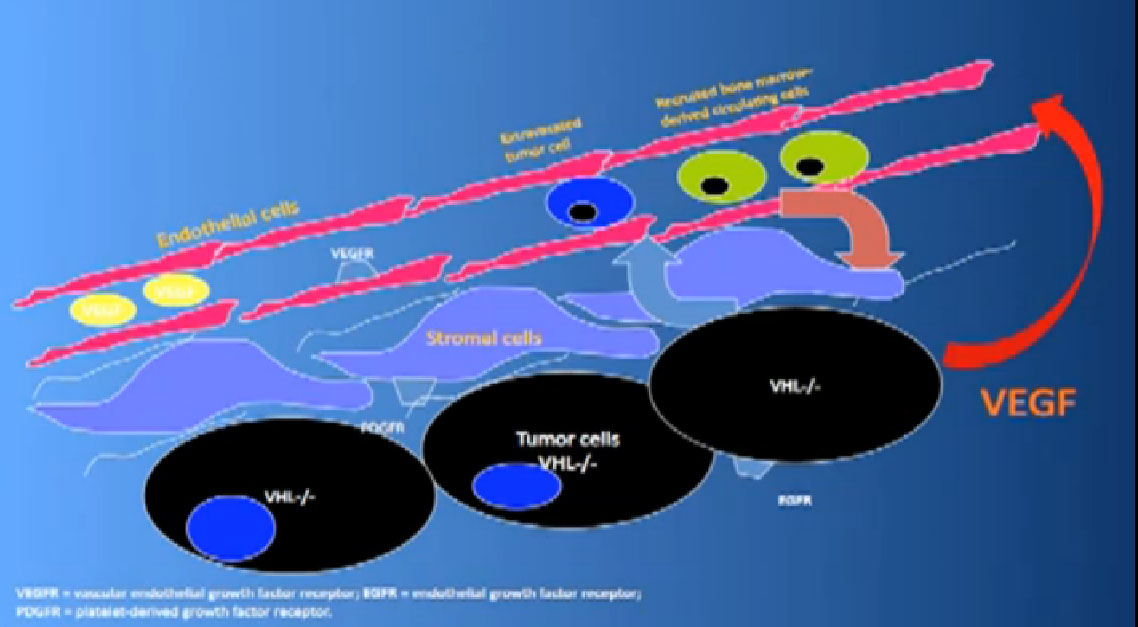
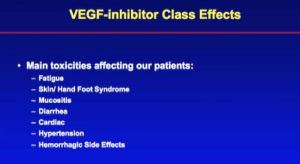
Let’s start first with the VEGF inhibitors, and follow with the mTOR inhibitors. The VEGF inhibitors, include Avastin (bevacizumab), an antibody treatment given by IV, and the TKIs, oral drugs, Sutent (Sunitinib), Votrient (pazopanib), Nexavar (sorafenib) and Inlyta(Axitinib). Their similar toxicities are called class effects.
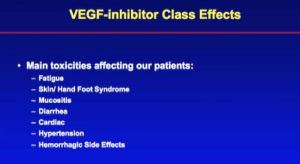
The effect we see in clinic and most often reported by patients is fatigue. Next are skin/hand foot sores, mouth sores, and diarrhea–daily monster diarrhea. Cardiac concerns, the biggest being hypertension; patients’ hemorrhagic effects don’t seem very big, but epitaxis, i.e., bloody nose is very common.
What is Hand/Foot syndrome? This is palmar plantar erthrodysesthesia, a medical term for painful palms and soles of the feet. Often with calluses form on the pressure points, even cracking. It can get very severe, so the patient is unable to use the hand or the foot, unable to walk. One of my patients had an acute reaction with Nexavar and within three days came to me in a wheelchair. Thankfully that kind of acute reaction is relatively rare. This type of skin toxicity manifests itself in the first 2-3 weeks of therapy, reaching a peak in the first couple of months of therapy.
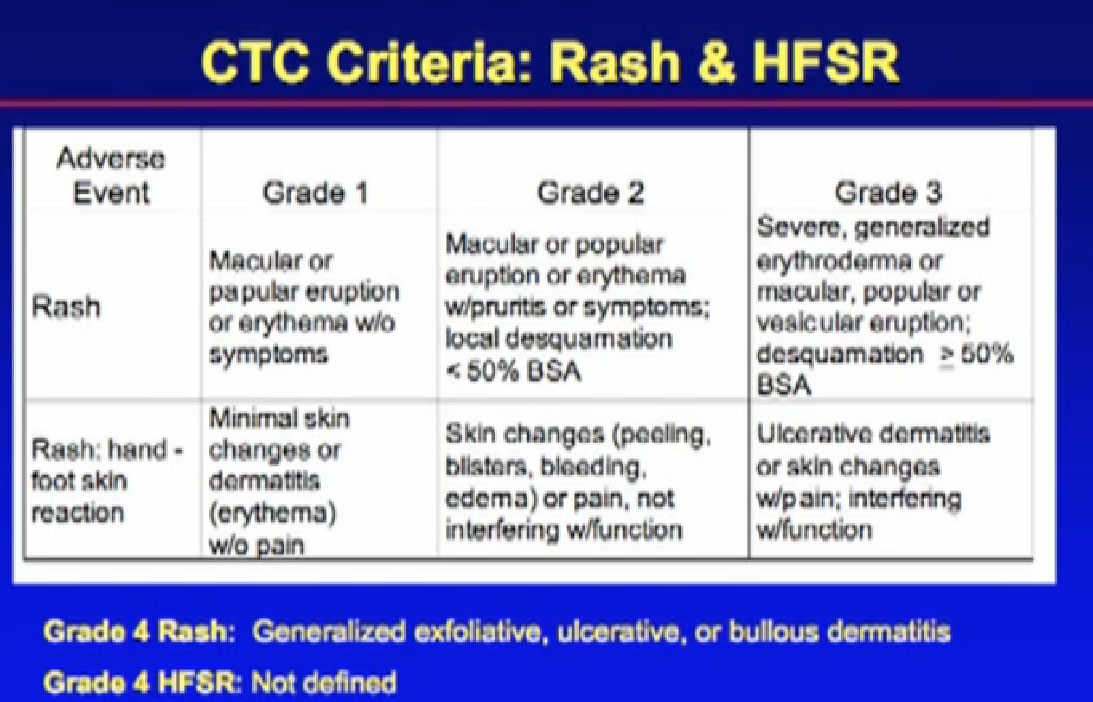
How do doctors talk about this? You have all heard doctors saying, “grade 1 toxicity, grade 2 toxicity” What does that mean?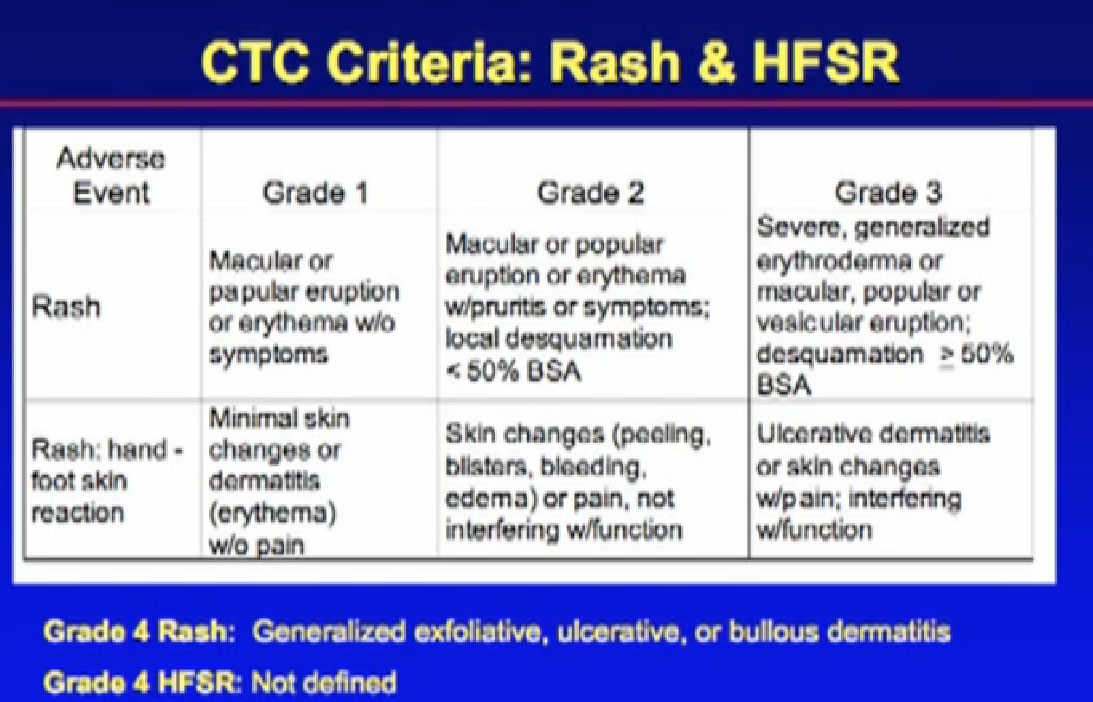
To standardize reporting, we use a common language—Common Toxicity Criteria—from the National Cancer Institute, and incorporated into clinical trials. Every doctor can grade the toxicity of a patient in the same way.
Grade 1 would be the mildest toxicity, an eruption, and macular/popular eruption, a bumpy patch. Grade 2 would be the eruption, the bumpy, and now itching, covering less than 50% of the body surface, and Grade 3 would be that eruption, with itching and covering greater than 50% of the body surface area.
For Grades 1 and 2 we use supportive care, and topical emollients and such. For the grade 3 toxicity, very severe, we might hold the drug, let the eruption go away, and potentially, lower the dose.” If it continued or returned, we might change the therapy. Same for Hand/foot Syndrome; Grade 1, minimal changes. Grade 2, more blistering, more peeling, more pain, but not really interfering with your daily activities. Grade 3 is means it interferes with daily activities; you can’t use your hands or feet, affecting your daily life. Same thing; grade 1 and 2, supportive care, and at grade 3, we would be more aggressive.
There is also actually a grade 4 toxicity, which is very extreme side effects and a grade 5, usually considered a side effect that resulted in death.
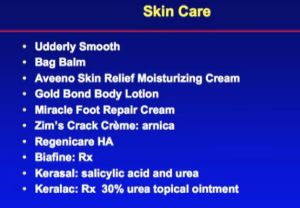
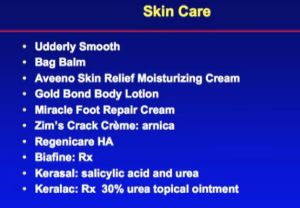
For supportive care we suggest Udderly Smooth, Bag Balm, Aveeno, non-allergenic emollients or creams; good skin hygiene, good foot hygiene, avoiding shoes with pressure points in them, pain medications, traditional pain medications. Some patients use Solarcaine spray, which numbs the surface of the skin.
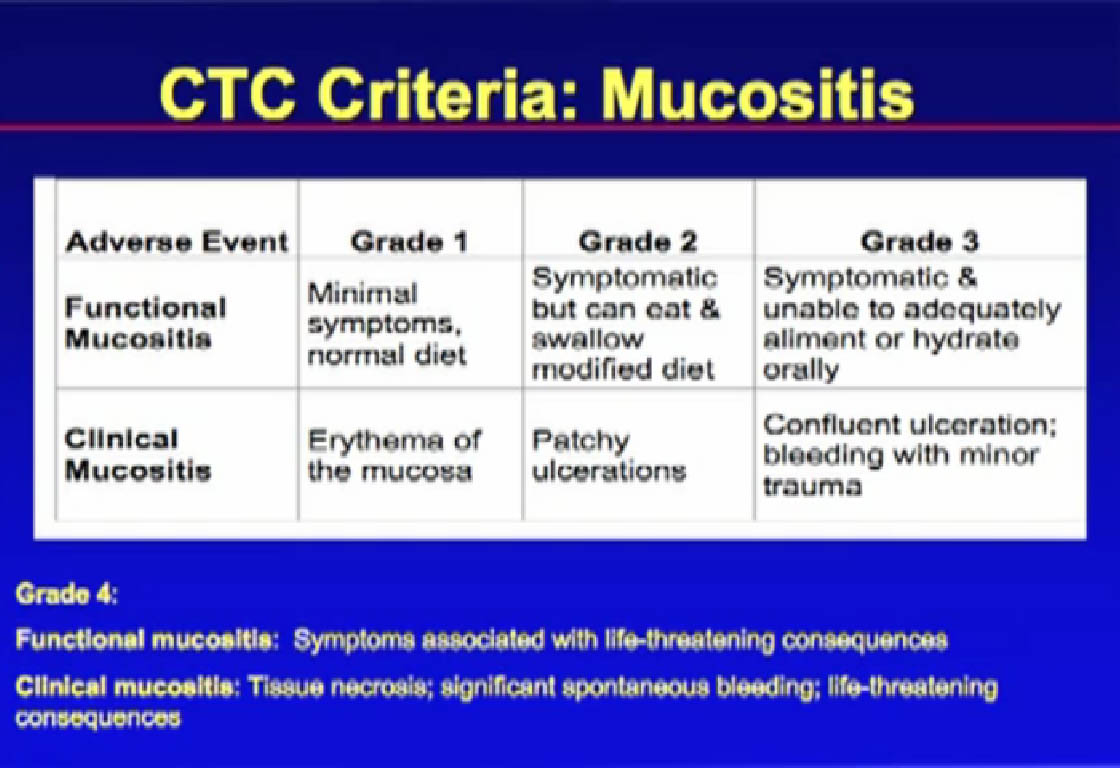
The next side effect, mucositis or stomatitis, those are mouth sores. We can do a mix of things–tap water or salt & soda mouthwash, that baking soda kind of mouthwash, change toothpaste, as some brands burn.
Lidocaine, such as dentists use can numb the mouth. We don’t want the mucositis to affect the patient’s ability to maintain hydration, the ability to eat, so again, monitor it.
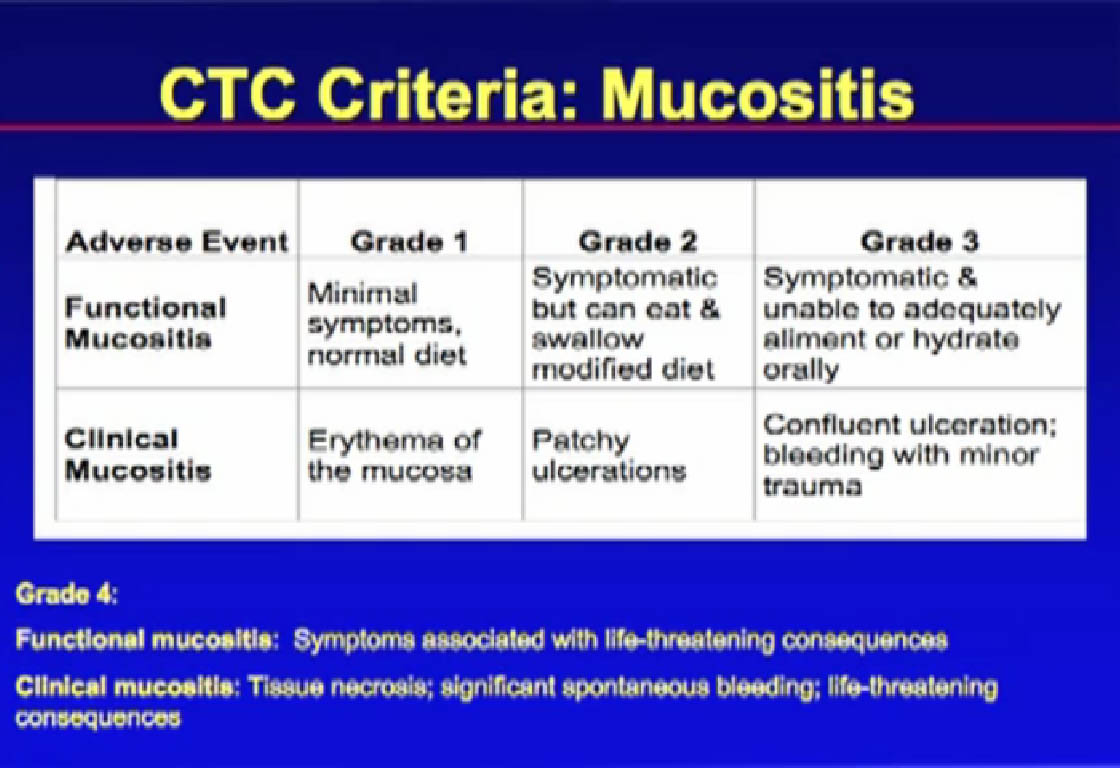
Grade 1; mild side effects–use all the supportive care. Grade 3, very symptomatic, can’t eat, can’t drink, very difficult, and we must consider holding the drug or lowering the dose.
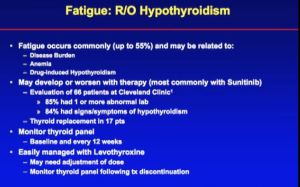
With Hypothyroidism fatigue is the major issue and with some of our drugs, fatigue occurs in 55% -65% of patients.
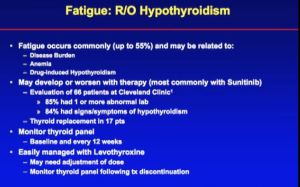
Fatigue has many possible causes, as it not one thing that causes fatigue in any one individual. Patients can have multiple causes at the same time, including the disease itself, anemia, lowering of the blood count from treatment, and pain medications.
We found the association of these drugs with low thyroid early on at the Cleveland Clinic. Many of these TKIs, at some level or another can affect thyroid function. Doctors need check thyroid functions in patients, especially if they have fatigue. This is something we can easily fix and put a patient on thyroid replacement therapy. Levothyroxine, a thyroid replacement therapy, may be used by a 1/3 or more of patients. Thyroid problems induced by these drugs is very common.
With thyroid issues we are constantly chasing TSH. It fluctuates constantly with these agents. My patients’ TSH is going up and down on their synthroid doses, very common. The graph shown here with Sunitinib therapy, shows the fluctuations of the TSH. If there is problem I am unable to control, I bring in a specialist, an endocrinologist.
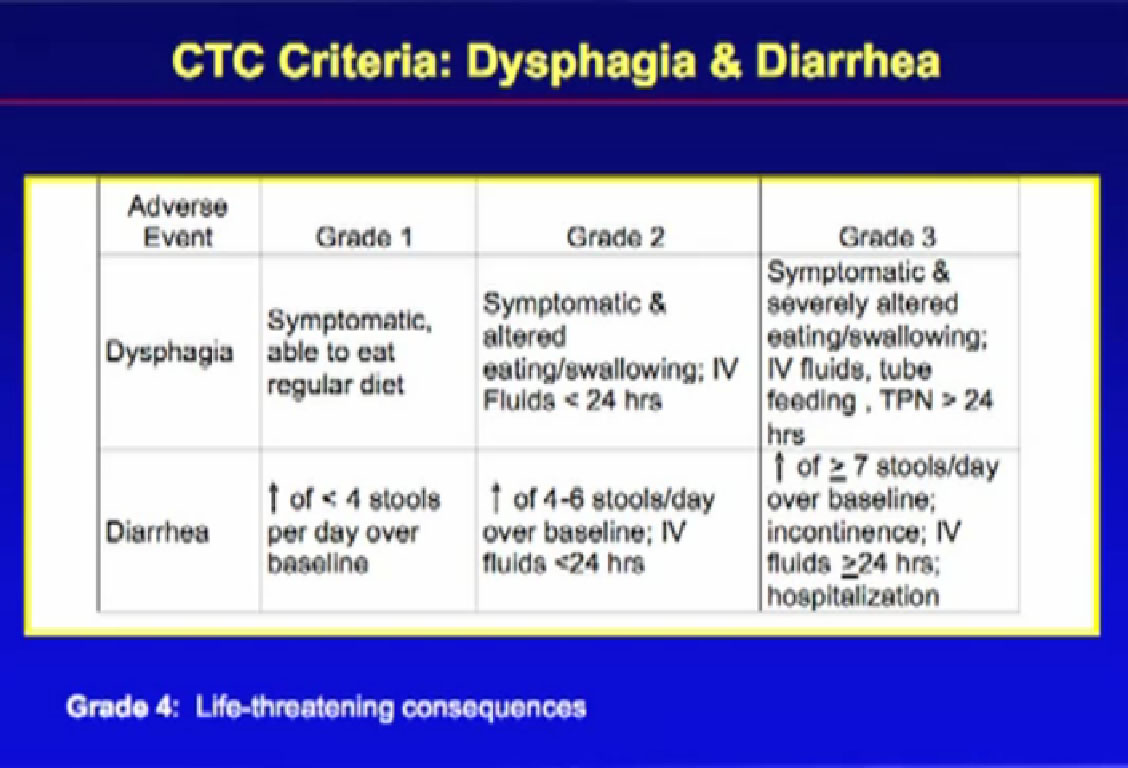
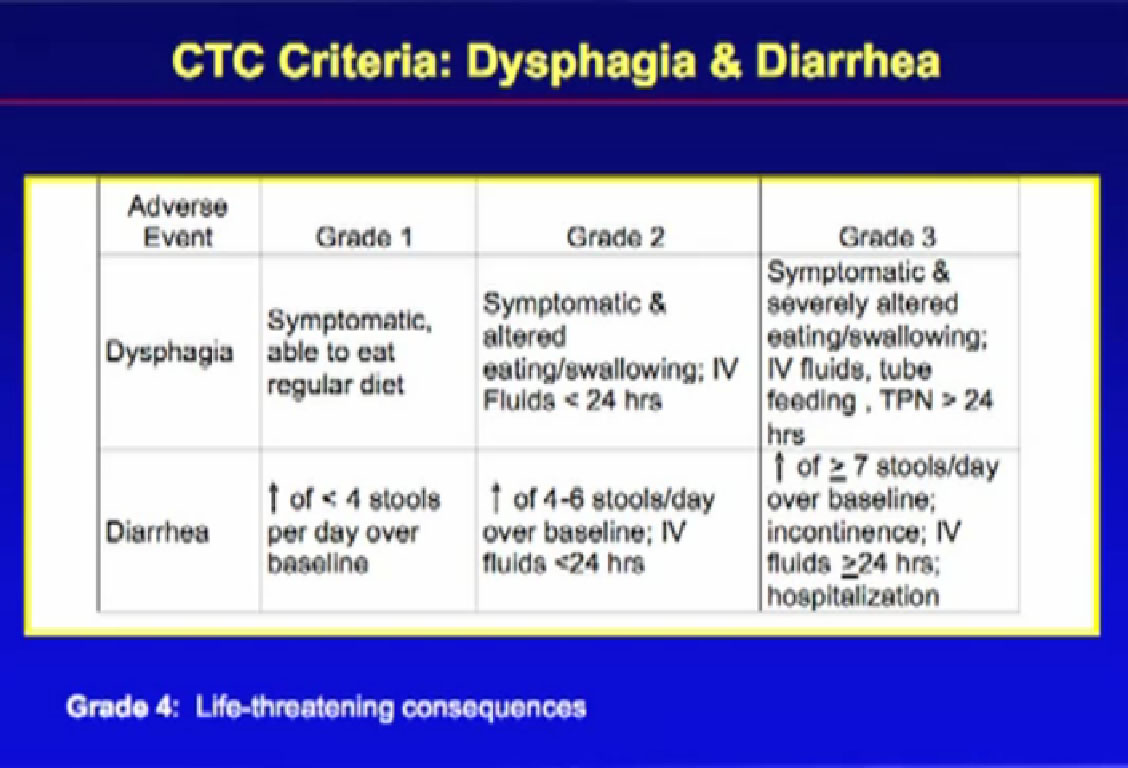
Next is dysphagia–difficulty in swallowing–and diarrhea, which is a big side effect, so will review diarrhea.
Grade 1 diarrhea is an increase of fewer than 4 stools over baseline, i.e., normal. In medical texts, it’s considered normal to have a bowel movement about every 36 hours. But if you are used to about 1 or 2 stools per day, and it goes up fewer than 4 more stools than what you normally have, that would be considered diarrhea. Diarrhea is NOT based on liquid stools, but the quantity of stools. So even if you were having formed stools, if you were stooling–having more stools—several times over your normal, that is diarrhea.
Grade 2 is when your stools increase more than 4-6 stools per day, incapacitating. Patients may become dehydrated, so we think about giving IV fluids. Grade 3 diarrhea is the very debilitating diarrhea. With the frequency of the stools, patients are becoming very dehydrated and may need lots of IV fluids, perhaps even hospitalization.
As to treatment, we try over the counter medications, Imodium or prescription meds like Lomotil, or different kinds of diets, the BRAT (bananas, rice, applesauce, toast and similar) diet, different foods. We get nutritionists and dieticians involved. We try to bulk up the food with fiber, with Questran (check with doctor), Fibercon, different fiber products, from over the counter. There are medications that the doctors can try, things like Octreotide or ?????, Sometimes we give pancreatic enzyme pills, that patients with pancreatic issues use. But most patients have grade 1 or 2; we’ll try to control it, not eliminate it. These patients will have diarrhea every day, but controlled with Imodium and Lomotil.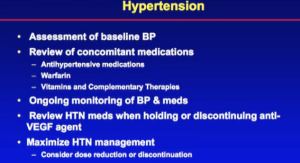
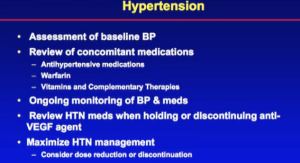
Hypertension is a classic side effect, almost an on-target effect of VEGF inhibition. It is currently being investigated to determine if hypertension can be seen as a biomarker of activity against the cancer. That may mean that patients who develop high blood pressure while in therapy may have a better chance of response to the therapy than those who do not.
We tell other doctors not to lower the dose of the cancer drug, as that is a good sign. Keep that going, but treat the high blood pressure. Do that with blood pressure drugs, the kind patients are already on.
If I have a patient who that is having difficulty, and we are using 2 or 3 blood pressure drugs, I will refer him to a nephrologist, a kidney specialist, who specializes in high blood pressures issues or a cardiologist to help me. But in general, it is very rare to find a patient who cannot be on these therapies due to blood pressure issues. If the patient is already on blood pressure medications, he is going to have troubles down the road. We identify that before starting the therapy, be proactive. Have the patient check their blood pressure daily, keep a diary, review that, have a plan so they can stay on their therapy.
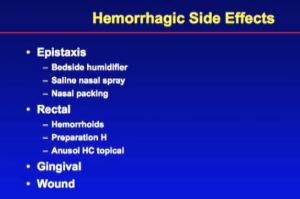
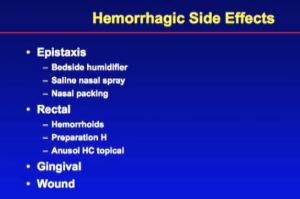
Epitaxis–bloody nose seems to happen quite a bit, especially when seasons change. The listed medications don’t have direct effect on the mucosal lining, but may when patients have inflammation., if they don’t make the blood is more thin. We use bedside humidifiers, Vaseline in the nose, nasal steroids and different agents to try to control it. I’ve only had one or two patients who had a major problem.
If you are predisposed to hemorrhoids , there may be more bleeding than usual. Try the topical products here, like Preparation H. Gingival bleeding, bleeding from the gums when you brush your teeth. Key thing that will interest surgeons is wound complications. If you are to have a surgical procedure, tooth extraction, or a surgical procedure that normally considered minor, you have to be concerned there could have complications with bleeding. Sometimes we’ll have the patient hold the medication for a few days before a minor procedure.
With a major surgical procedure, the literature is very controversial about the length of time, generally a few days, but that is at the discretion of the surgeon, and their comfort level. You would resume the medication once there was appropriate wound healing. Usually the surgeon will visit with you a week or 10 days, and remove staples and that would be a good time to resume.
A lot of side effects and it sounds bad, but I share some hope here. Tolerance may develop with long-term use. This is information from Nexavar from the original trial. The first, HFSR, the hand/foot syndrome is shown with the axis as cycles, 1-5, a month of therapy. The high peak that patients seem to have in HDFS is in the first cycle and fewer as the weeks go by, they develop resistance. Same with the skin rash; same with diarrhea, hard in the first cycle, more controlled in the end. The fatigue is similar. So a tolerance can develop, but you have to fight through the side effects.
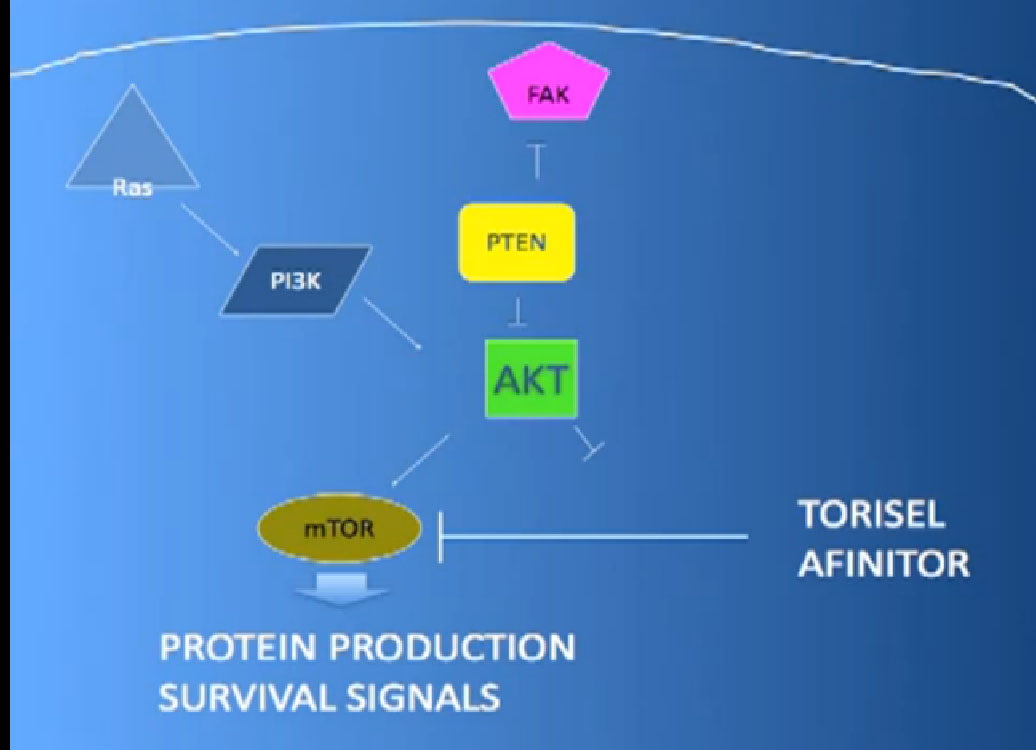
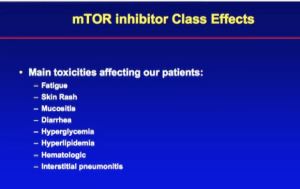
Now about the mTOR inhibitors. We have Torisel or temsorilimus, a IV weekly medication and Afinitor or everolimus, the oral medication. Just as with VEGF inhibitors, these have class effects associated with both.
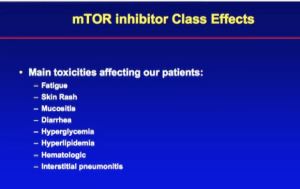
We see fatigue, skin rash, but no hand/foot syndrome. It’s not that severe life/quality of life syndrome that we see with the VEGFs inhibitors. You can get a mucositis, less severe that the VEGF inhibitors or diarrhea, but that is essentially it. You do not get the high blood pressure issues as with the VEGF inhibitors. Generally patients feel that the mTOR inhibitors are more tolerable, less difficult, less severe side effects than the VEGF inhibitors.
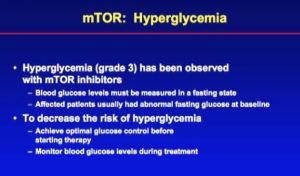
Unique about this class are hyperglycemia–raising of the blood sugar and elevation of cholesterol. If you have diabetes while taking mTORs, you may have to adjust up your diabetes medications. If you don’t have diabetes, it can sometimes cause a drug-induced diabetes, that requires medication, and is reversible upon stopping the drug. It is reversible side effect, but we have to plan for it.
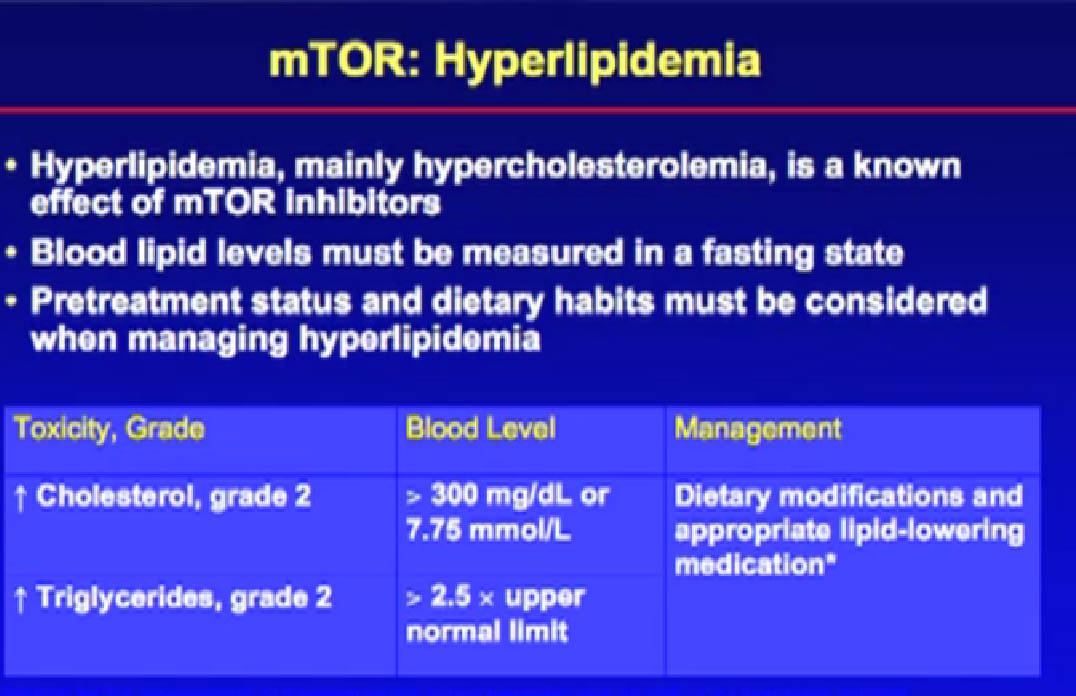
Hyperlipidemia–elevation of cholesterol levels. I will check cholesterol levels every two months with patients on mTOR inhibitors. If we start to see it rise, we start them on therapy. Many of my patients are already on statins, lipid lowering medications, but it doesn’t seem much of a problem in them. But if a patient isn’t already on, they can develop this.
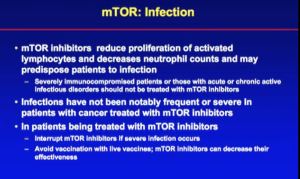
Hematologic effects. The mTOR inhibitors can lower blood counts, create problems with white blood cell counts, and infections, more than VEGF inhibitors. As a class, mTOR inhibitors are not just used to treat kidney cancer. Long term, and in Europe, they have been used as immunomodulators for transplant patients. They change the immune cells in the body to prevent rejection of organs. For patients with kidney cancer, we change doses, but they can create changes in the immune system and put patients to be at risk for infections, like pneumonia. Doctors have to watch for infections when on Torisel or Afinitor.
A unique side effect to this class is interstitial pneumonitis–inflammation of the lungs. If it occurs, and causes symptoms of coughing or shortness of breath, we need to consider discontinuing therapy. More details on that.

A skin rash with Torisel is usually on the torso. We use a topical crèams, emollients with Benedryl. We try to avoid using steroids, as this drug already has an immune effect and we don’t want to add to it. With a patient who has grade 2, less than 50% of the body affected in a skin rash, I sometimes get a dermatologist to help. If the rare patient develops the grade 3, with more than 50% body surface affected, I would have to consider stopping the medication.
Hyperglycemia has been seen with both the mTOR agents, and we need to monitor blood sugar. Sometimes that means making the patients get a blood monitor, to check their blood sugar medications at home, or start diabetes medication.
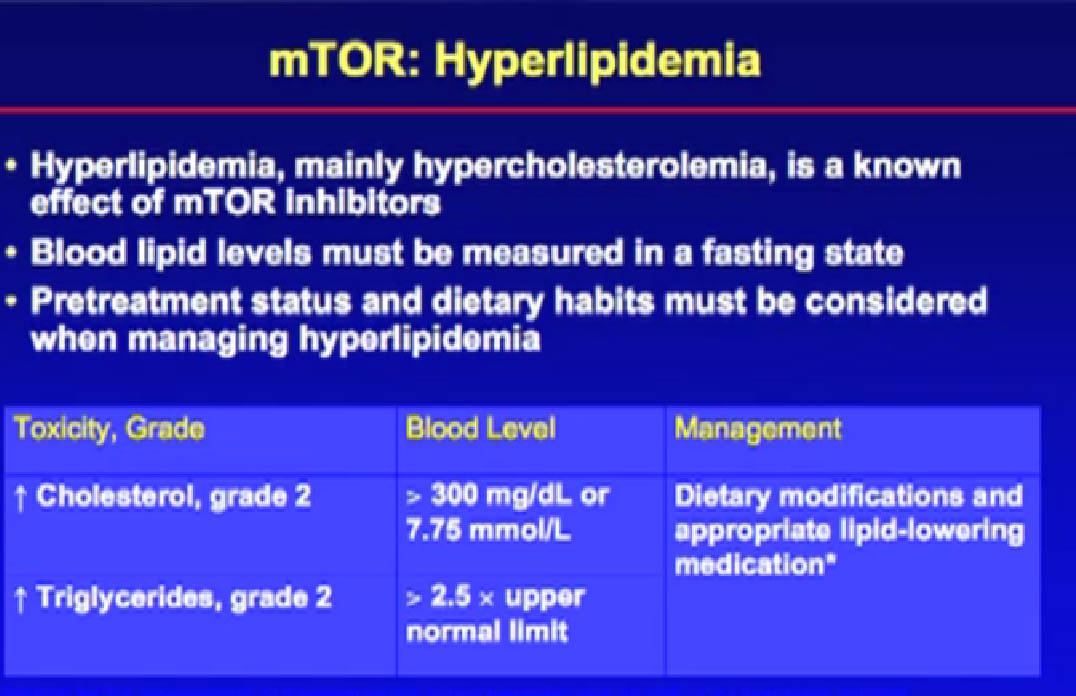
Again you can see elevations in triglycerides and cholesterol requiring patients to start on lipid-lowering medications. Those are both reversible when you stop the medication.
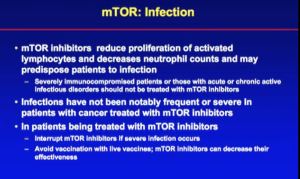
We talked about infection. There is a chance of infection with the mTOR inhibitors, so we need to be on alert for that.
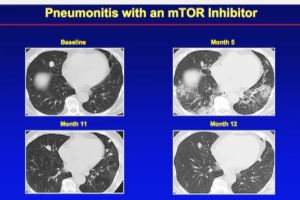
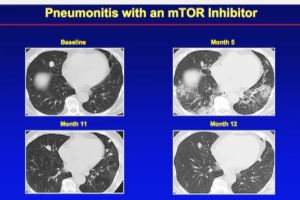 Seen here are CT scans of interstitial pneumonitis: in month five there was a development of this nasty-looking infiltrate in the CT scans. That scares everyone when we find this on a CT scan. It could be ones, one; an atypical pneumonia, two; interstitial pneumonitis, a drug side effect, or the cancer. Sometimes, we have to refer patients to a lung specialist for a bronchoscopy to determine what it is. In this case, it was a drug effect, not an infection, and it was not cancer. It was the actual drug inflaming the lungs.
Seen here are CT scans of interstitial pneumonitis: in month five there was a development of this nasty-looking infiltrate in the CT scans. That scares everyone when we find this on a CT scan. It could be ones, one; an atypical pneumonia, two; interstitial pneumonitis, a drug side effect, or the cancer. Sometimes, we have to refer patients to a lung specialist for a bronchoscopy to determine what it is. In this case, it was a drug effect, not an infection, and it was not cancer. It was the actual drug inflaming the lungs.
They stopped the drugs, they gave a little burst of steroids, it went away. Later they rechallenged the drug, and the patient went back on the drug, without further recurrence of the interstitial pneumonitis. If I had a patient with interstitial pneumonitis, I would find it very hard to put them back on the therapy. I show this to demonstrate that it is a reasonable side effect to expect, and it is reversible. It manifests itself as an x ray finding or as a cough.
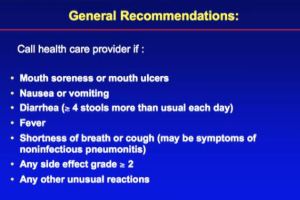
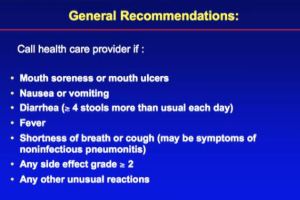
The general recommendations are as shown. Call if there is any side effect which you are uncomfortable with. It is better to call early so you can intervene on it before it becomes a problem.
END of LECTURE: Questions follow from patients and caregivers.
Patient responses; Patient suggests Rock Alum in the case of mouth sores.
4 Archway macaroon cookies, twice a day
Capcesin for foot sores
Doctor agrees that patients have much to offer help with some symptoms.
Questions re coconut oil, to be used for mouth sores; Doctor had not heard of that.
Side effects do get better, says patient, asking about taking acidodolphodus; doctor agrees that pro-biotics, yogurt, is helpful, perhaps to change gut flora.
Question re Zometa as it is used with Sutent; Zometa has benefit in reducing skeletal related issues, and would be beneficial with all the drugs, says doctors.
As to difficult skin issues, doctors suggest the use of anti-fungals and consults with a dermatologist.
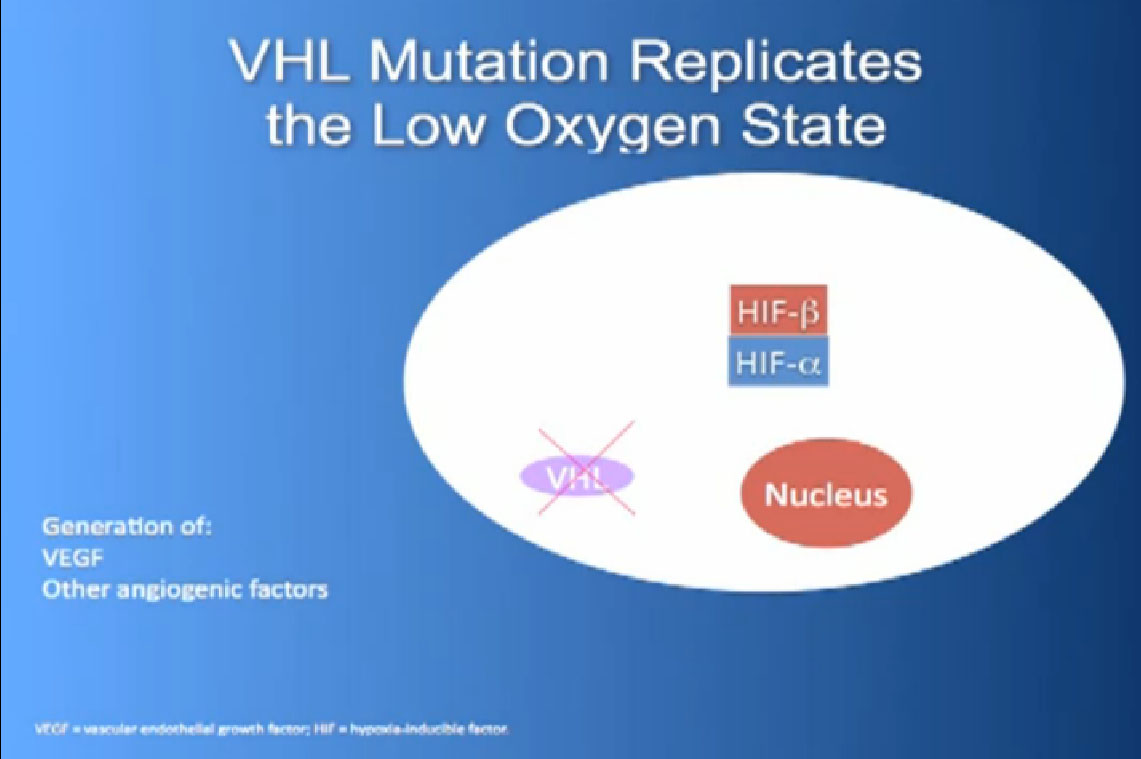
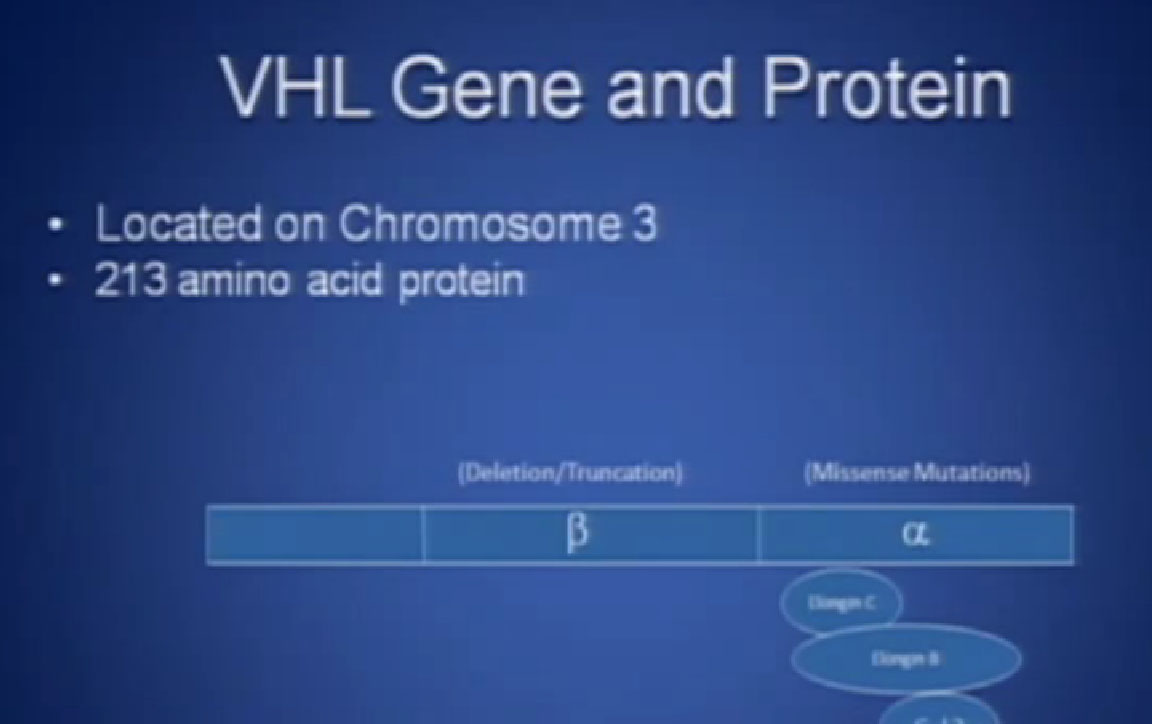 Slide 2: This is not to scale; it is 213 amino acids long and for the scientists in the audience, that is mercifully short, and it also has three exons in or three parts, or easier to study than most, but obviously still hard to study.
Slide 2: This is not to scale; it is 213 amino acids long and for the scientists in the audience, that is mercifully short, and it also has three exons in or three parts, or easier to study than most, but obviously still hard to study.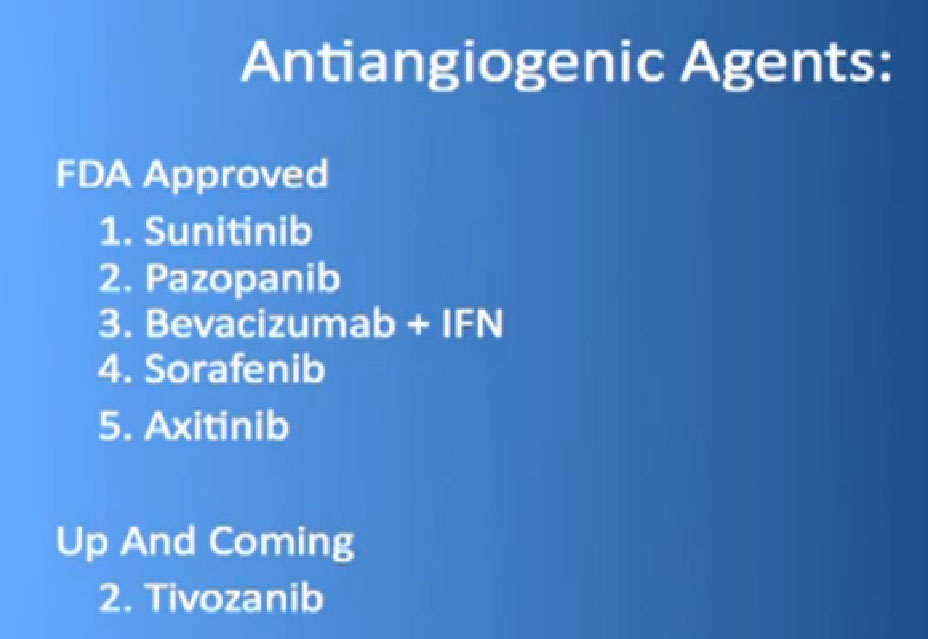 So the “blood vessel starving” are the five antiangiogentic therapies we currently have are listed here, and I am going to go through each of these in details.
So the “blood vessel starving” are the five antiangiogentic therapies we currently have are listed here, and I am going to go through each of these in details.